What is Meaningful Use?
The U.S. government introduced the Meaningful Use (MU) program as part of the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act to encourage healthcare providers to show "Meaningful Use" of a certified Electronic Health Record (EHR) system. Healthcare providers must meet and attest to annual Meaningful Use metrics and performance measures in order to receive full reimbursement from Medicare, the largest healthcare payer in the United States.
The Meaningful Use provisions are part of larger goals of the HITECH Act (2009) and the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which changed the way physicians are paid by Medicare and Medicaid. MU EHR requirements initially unfolded in three stages beginning in 2011 and are now part of the MIPS program, a Quality Payment Program that emphasizes value over volume for healthcare services.
The Meaningful Use program, also known as the Centers for Medicare & Medicaid Services (CMS) EHR Incentive Program was established to create a healthcare infrastructure that improves the quality, safety and efficiency of patient care in the United States.
Why is Meaningful Use in healthcare important?
Meaningful Use is an important metric for healthcare organizations to meet so they can receive full payment for services from CMS and coordinate care for their patients across healthcare providers such as labs, pharmacies, ambulatory centers, specialists, hospitals, and primary care physicians.
As a cornerstone of US healthcare regulations, the Meaningful Use program has helped drive the adoption of healthcare technology, specifically electronic health records systems like athenaOne®. MU requires healthcare information to be stored digitally in EHRs (also known as electronic medical records) instead of paper records, to have the ability to communicate with other healthcare information technology (interoperability), to provide patients with access to their healthcare information, and to protect patient information security and privacy, strengthening provisions in the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
The Meaningful Use regulations require healthcare providers from small physician practices to large hospitals and healthcare systems to adopt certified EHR technology (CEHRTs) and to demonstrate that they are using them in accordance with the metrics CMS establishes. Healthcare providers report on their meaningful use of EHRs annually through a process called attestation.
The Meaningful Use program was always about more than mere digitization of paper medical records. Of all the benefits of Meaningful Use, the overall value of the program is that it helps foster a safer, more efficient way to practice medicine while also working to control healthcare costs.
What are the goals of meaningful use of EHRs?
The Meaningful Use program consists of measures, requirements and timelines to satisfy a valuable set of goals: smooth, accurate data-sharing among healthcare providers, greater privacy, security and patient access to data, and a higher quality of care for all patients. The goals of the Meaningful Use program are outlined in the HITECH Act to transform the US healthcare system:
- Improving quality, safety, and efficiency of healthcare in the US
- Engaging patients in their care
- Increasing coordination of care
- Improving the health status of the population, and
- Ensuring privacy and security.
Are there Meaningful Use incentives or penalties?
Initially, to qualify for Meaningful Use incentive payments, eligible healthcare providers had to not only adopt an EHR, but also show that they are "meaningfully using" their electronic health records systems by meeting a number of objectives designed to positively impact patient care. Beginning in 2015, physicians who fail to demonstrate Meaningful Use of an EHR system as defined by annual CMS metrics are penalized and may receive reduced Medicare and Medicaid reimbursements.
Not meeting Meaningful Use requirements can have a dire impact on a healthcare organization’s bottom line, so physicians and other providers take Meaningful Use seriously and work closely with their EHR software provider to ensure they are meeting and properly reporting their MU performance to avoid a significant loss of revenue.
What has replaced Meaningful Use in healthcare?
Interoperability was one of the core tenants of Meaningful Use. So much so that in 2019, The Center for Medicare and Medicaid (CMS) changed the program name from Meaningful Use to Promoting Interoperability to reflect its ongoing commitment to connectivity, patient data access, and system-wide health information exchange. Even though Meaningful Use is now known as the Promoting Interoperability (PI) metric in MIPS, since it has been a staple of CMS regulations since the HITECH Act, many people still use the term Meaningful Use. When we define Meaningful Use in 2024 and beyond, it refers to the EHR interoperability requirement as part of the MIPS program.
With the passage of the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, the goals and requirements of the Meaningful Use program became part of the Merit Based Incentive Payment System (MIPS) model. The Center for Medicare & Medicaid Services (CMS) consolidated three CMS Quality Programs into a single program to improve US healthcare and streamline regulations. Meaningful Use is now part of the Promoting Interoperability pillar of MIPS and remains an important performance measure that healthcare organizations must strive to meet.
So, although MU is no longer a standalone CMS program, using certified EHR technology (CEHRT) and meeting the Meaningful Use interoperability requirements to coordinate care is an important part of complying with MIPS regulations and maximizing your healthcare organization’s Medicare Part B and Medicaid reimbursements.
How do I meet Meaningful Use requirements?
In order to meet the Meaningful Use requirements under the MIPS program, healthcare providers need a complete, fully certified EHR, and a healthcare IT partner with the advanced processes, resources, experience and services to assist healthcare organizations in successfully achieving and reporting on Meaningful Use Promoting Interoperability Performance metrics annually.
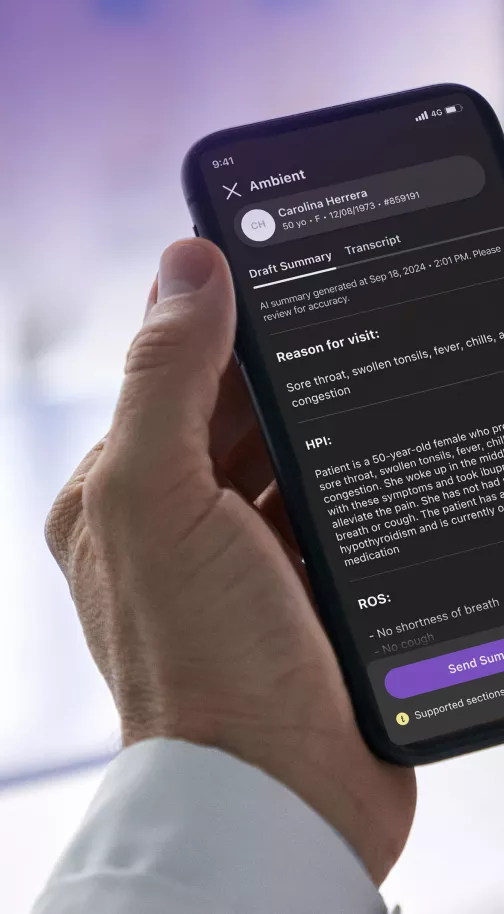
athenaOne® is a cloud-based certified electronic health records system that meets all data privacy and security, patient access, and interoperability requirements under the MIPS Meaningful Use provisions. It also integrates medical coding and billing, claims authorization and management, and patient engagement tools such as appointment reminders, patient portal, and telehealth into a single healthcare software solution that you and your patients can access from any computer or mobile device.
At athenahealth, our team of healthcare IT professionals has helped over 150,000 providers across the United States demonstrate Meaningful Use of EHRs and maximize their Medicare and Medicaid reimbursements from CMS. As healthcare regulations change and performance metrics become harder to meet, athenaOne® automatically updates to ensure you are staying on top of requirements and have a dashboard to monitor the health of your practice or larger healthcare organization at a glance.
Reach out to one of our healthcare IT specialists to learn more about how athenaOne® for small- and medium-sized healthcare practices, clinics, and hospitals or athenaIDX for larger enterprise healthcare organizations can help you demonstrate Meaningful Use and meet other MIPS Performance Index requirements – all while offering greater efficiency in your workflows and engagement with your patients.