Article
Where are the patients at highest risk for COVID-19?
By Lia Novotny | May 22, 2020
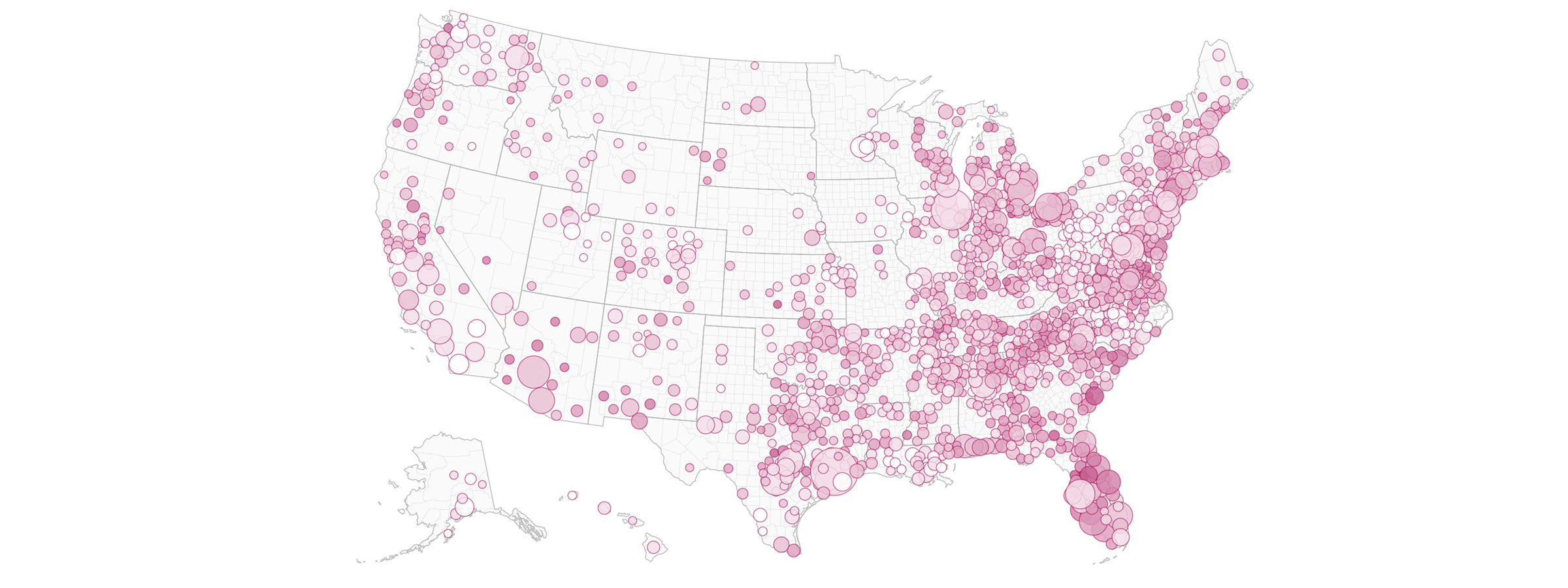
These high-risk conditions are not evenly distributed throughout the country — in fact, there are clear geographic areas with higher-risk populations. So, what can the national healthcare system and the federal government do to support these areas and protect their populations?
The first step is identifying where patients at greatest risk are concentrated. To that end, athenahealth created a COVID-19 dashboard on high-risk patients, drawing upon data from our national, connected network of providers.
Organizations form coalition to share data and flatten the curve
We’ve also joined other healthcare, technology, non-profit, and academic organizations participating in the COVID-19 Healthcare Coalition, which was designed to leverage the data and expertise of participants to flatten the pandemic’s curve, slowing the spread so that the healthcare system is not overwhelmed. The coalition is co-chaired by Jay Schnitzer, M.D., chief medical and technology officer at MITRE, and John Halamka, M.D., president of Mayo Clinic Platform.
The coalition consolidates and analyzes real-time data to inform decisions regarding COVID-19 policy decisions and the distribution of healthcare resources, with the purpose of protecting populations and preserving the healthcare delivery system in the U.S.
Private data for public good
The ability to consolidate and analyze de-identified national data on these conditions is fairly unique, making the athenahealth COVID-19 high-risk dashboard a crucial element of this effort. Using electronic health record (EHR) and billing data at the county level, this dashboard reports on the percentage of patients who are aged 65 and over or have been diagnosed with any of nine chronic conditions associated with severe illness in COVID-19 patients, providing information that can and should be crucial to making smart resource allocation decisions as the pandemic continues.
“EHR companies like ours have data that could help solve a lot of public health issues, especially when we partner with the public sector,” says Bethany Sheridan, Ph.D., Senior Manager, Research and Insights at athenahealth. “That was actually true way before COVID, but people are really starting to see it now.” One positive outcome of the pandemic may be a greater understanding of how important it is from a public health standpoint to share and analyze this kind of population-level information.
Greatest risk often aligns with lowest level of healthcare resources
Of the 2,208 athenahealth patients in Pratt County, Kansas, nearly half are over the age of 65 and 73 percent (1,600 patients), have one or more of these high-risk conditions; 44 percent of athenahealth patients fall into both categories. The local regional medical center and hospitals in neighboring counties are not set up to treat hundreds of severely ill patients at once — nor should they be, since they are built to meet the typical needs of their population. However, if a significant number of these patients were to contract COVID-19 and develop severe illness, it could very quickly overwhelm the county’s existing resources.
This scenario is repeated in countless counties across the country, often in rural areas with fewer local hospital beds and providers or in areas with large minority and low-income populations at high risk of contracting COVID. Of the 3,600 athenahealth patients in Llano County, Texas, 69 percent have high-risk co-morbidities that put them at greater risk of severe illness should they contract COVID-19; 68 percent fall in this category in Sumter County, Florida (which also has the highest median age in the country); 75 percent in Dougherty County, Georgia, and the list goes on. Population density is relatively low in many of these counties. Median annual income hovers around $50,000, and the poverty rate tends to be well above the national average .
By and large, health systems, medical providers, and ICU beds are concentrated in urban areas with higher population density, leaving high-risk patients in other areas notably vulnerable. The implications for health outcomes, strain on the healthcare delivery system, and local economies is likely to be extreme.
Policy implications and resource distribution
In keeping with the Coalition’s goals, this kind of data analysis can be a springboard to policy decisions aimed at mitigating negative consequences. First and foremost, this kind of information could help guide social distancing efforts and other community actions to slow the spread of COVID-19 and protect the most vulnerable.
Second, understanding where the most vulnerable patients are may help guide testing efforts, perhaps leading national or local government agencies to set up mobile testing sites in areas with large numbers of high-risk patients. The natural corollary would be aggressive contact tracing and isolation procedures based on test results.
Finally, this information can and should inform national and regional decisions regarding allocation of healthcare resources. Areas with a large concentration of high-risk patients could be targeted for delivery of ventilators and stockpiles of personal protective equipment (PPE). Overflow locations for treatment and isolation could be identified in advance. And providers from other areas of the country could be on call to deploy to these areas in the event of a COVID-19 surge. With data like this, local providers can dig into the risk of their particular patient populations.
athenahealth is helping our customers do just that by providing additional data on which patients in their panels are at highest risk. “We’re actually using this data to help our customers figure out which patients they should reach out to right now with extra information and support,” says Sheridan. “In a way, this is nothing new. Clinicians have been trying to get more consistent in how they care for patients with diabetes or hypertension for years now – it just so happens that some of the risk factors for severe illness with COVID are those same ones.”
In the long term, these findings highlight an underlying truth: there are significant inequities in our healthcare delivery system and in health itself. At some point, it will be important to ask why these health conditions are so much more prevalent in areas that are rural, lower income, or have higher concentrations of minorities.
Addressing the upstream factors impacting overall health in these areas in order to lower risk should be an important aspect of being prepared for the next pandemic, as well as benefiting patients today. COVID-19 may help focus resources on the population health work that should have been happening all along.
“COVID has brought some really alarming health disparities by race and socioeconomic status to the forefront, all at once,” observes Sheridan. “We’ve known for a long time that better chronic condition care disproportionately helps disadvantaged groups, and there seems to be a renewed sense of urgency right now.”
Lia Novotny is contributing editor to athenahealth's Knowledge Hub.






