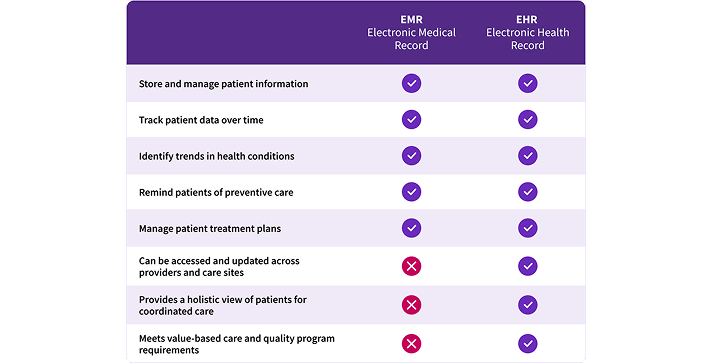
The critical difference between EMRs vs EHRs
If you’re struggling to understand the difference between an electronic medical record (EMR) and an electronic health record (EHR), you’re not alone. Many healthcare professionals and organizations face confusion due to how often these terms are used interchangeably. While both systems share certain characteristics, they differ in their capabilities and scope of use, especially when it comes to interoperability and data exchange.
This article explores the definitions of EMRs and EHRs, their differences, and their roles in modern healthcare delivery. We’ll also discuss the importance of Certified Electronic Health Records Technology (CEHRT) in supporting quality programs and value-based care, and why moving from a siloed EMR to a connected EHR can make a difference for your medical practice.
What is an Electronic Medical Record (EMR)?
An electronic medical record (EMR) is a digital version of the paper charts that healthcare providers traditionally used to document patient care. It is used by clinicians to store and manage patient information within a single healthcare practice. EMRs typically include a patient’s medical history, treatment plans, diagnoses, medications, and test results, all stored digitally for quick access and improved efficiency.
EMRs allow healthcare professionals to:
- Track patient data over time
- Identify trends in health conditions
- Remind patients of due preventive care (such as vaccinations or screenings)
- Manage patient treatment plans within the practice
However, one of the limitations of an EMR is that it is often confined to a single practice or healthcare provider. EMRs don’t automatically share patient data with other healthcare organizations or specialists, meaning that if a patient visits another doctor or requires specialized care, their medical records must be physically or digitally transferred. This can lead to fragmented care and delayed decision-making due to the lack of real-time data sharing. And while digital faxing can help solve for this lack of native data interoperability, that means that information from other providers doesn’t integrate into your patient records where and when you need it.
What is an Electronic Health Record (EHR)?
An electronic health record (EHR) builds on the foundation of an EMR but with a critical improvement: it is designed to be shared across multiple healthcare settings. EHRs allow patient records to automatically move with the patient as they seek care from different healthcare providers —whether that’s a specialist, a lab, or a hospital.
EHRs include the same patient data found in EMRs, but create a more comprehensive picture of a patient’s health by incorporating this information from more than one provider:
- Patient medical history
- Treatment plans
- Medication lists
- Diagnostic tests
Importantly, EHRs are interoperable, meaning that they can be accessed and updated by various authorized healthcare providers at different care sites. This allows for more coordinated, patient-centered care, as every clinician involved in a patient's care has access to the most current and complete version of their health records – as long as those providers are also using EHRs. To participate in many quality programs from the Centers for Medicare and Medicaid Services and adhere to many commercial payers’ increasing use of value-based care contracts, medical practices find they need an EHR’s capabilities beyond the digitized health record of an EMR.
What's the Difference between an EMR and an EHR?
The short answer is that every EHR is an EMR, but not all EMRs are EHRs. While both EMRs and EHRs store digital patient records, the key difference lies in interoperability—the ability to exchange data between different healthcare organizations and providers. EMRs are typically used within a single practice and do not easily share information with other healthcare systems. In contrast, EHRs are built to be shared across practices, health systems, and a wider array of healthcare providers, allowing patients’ health data to follow them as they see different specialists or go to multiple healthcare facilities.
What are the Benefits of an EHR vs an EMR?
There are several key benefits that come with using an EHR over an EMR system:
- Improved Care Coordination: EHRs can be accessed by multiple providers, allowing for better coordination of care when a patient sees specialists, visits hospitals, or needs urgent care. More connected care helps avoid potential drug interactions, duplicate tests or missed diagnoses.
- Better Patient Outcomes: With the ability to more easily share information, clinicians can make more informed decisions, often in real time. Quicker diagnoses, more accurate treatment plans, a more holistic picture of a patient’s health – all of these can help improve outcomes.
- Increased Efficiency: EHR systems streamline clinical workflows by automating routine tasks like appointment scheduling, prescription management, and documentation. Medical coding and payer information is often built-in to help clinicians document quickly and understand what an insurance plan will cover.
- Data Accuracy and Accessibility: EHRs can include additional tools through third party integrations or may natively include AI-powered capabilities for voice-to-text dictations, ambient listening, generative-AI clinical notes summaries, OCR scanning of insurance cards, automatic insurance verification, and more.
- Support for Value-Based Care: EHR systems, especially CEHRTs, track quality metrics and patient outcomes, making it easier for healthcare providers to measure and improve care. Some, such as athenaOne, have built in connections to automatically submit quality program metrics, streamlining reporting and program requirements.
Is athenaOne an EMR or an EHR?
athenaOne is an EHR system. It stores and manages patient health data across various healthcare settings, enabling clinicians to provide coordinated care by accessing up-to-date information. athenaOne is interoperable, meaning it can easily exchange patient data with other healthcare providers and organizations, making it a crucial tool for practices that wish to provide comprehensive care to their patients. As a CEHRT, athenaOne also supports compliance with quality programs and value-based care initiatives.
You may have heard people refer to athenaOne or athenaClinicals as an EMR out of habit. That’s because EMR was the original term when paper health records were first digitized. Since then, the term EHR was introduced to distinguish first-generation, single-location EMRs from electronic health records designed for information sharing across care sites. With extensive interoperability built in, athenaOne’s clinical capabilities are properly referred to as an EHR, with the care coordination advantages that term connotes.
What's the Difference between an EHR and a Patient Portal?
A patient portal is an online platform where patients can access their personal health information, communicate with healthcare providers, request prescriptions, schedule appointments, and view lab results. While patient portals can be a component of an EHR system, they are not the same thing.
- EHR: A system used by physicians and healthcare providers to store and share patient records and medical history.
- Patient Portal: A tool that gives patients access to their own health data, usually derived from the EHR, allowing them to engage more directly with their healthcare.
The EHR stores and manages clinical data, and the patient portal provides access to some of that data to patients, allowing them to interact with their doctors and access their own medical records. Clinicians access the EHR directly through their log-in, while patients use patient-friendly specific views through the patient portal or mobile app. Patients only see what doctors make accessible to them, such as test results, care plans, and answers to patient questions.
Are All EHRs Certified Electronic Health Record Technologies (CEHRT)?
Not all EHRs are Certified Electronic Health Record Technologies (CEHRT), but to participate in certain government healthcare programs—such as the Medicare and Medicaid Promoting Interoperability Programs—healthcare providers must use a CEHRT. These certified EHR systems meet specific technical standards for interoperability, security, and data exchange, ensuring that patient records can be shared seamlessly across systems and institutions while protecting patient privacy.
CEHRTs are crucial for healthcare providers to engage in quality programs and value-based care, which rely on accurate, up-to-date health data to improve patient outcomes. By ensuring that data is shared across different providers and settings, CEHRTs facilitate better care coordination and help improve both the efficiency and effectiveness of healthcare delivery.
athenaOne® is a CEHRT with immediate access to 160K+ clinicians on the athenaOne network1 plus more than 277,000 nationwide clinical integrations immediately available to athenaOne customers, including direct connections to labs, imaging centers, pharmacies, and more.2 and immediate access to over 160,000 healthcare providers on the athenahealth network.
The Shift from EMRs to EHRs
The American Recovery and Reinvestment Act (ARRA) of 2009 played a pivotal role in the nationwide transition from paper charting to electronic medical records (EMRs). As part of this legislation, healthcare providers were required to adopt EMRs by January 1, 2014, to ensure better patient care coordination and reduce administrative inefficiencies. EMRs contain records of a patient's care within a particular practice or institution. However, ARRA’s reach extended beyond the adoption of EMRs to encourage the creation of interoperable electronic health records (EHRs) that could facilitate secure, real-time data exchange across healthcare settings.
This initiative was further supported by the 2015 MACRA law, which, through its Quality Payment Program (QPP), incentivizes healthcare providers to adopt EHRs that can communicate with other systems across various healthcare entities, such as hospitals, labs, pharmacies, and other clinicians.
The first generation of electronic medical records (EMR) met the needs of the 2009 ARRA law. But now, with the introduction of MACRA and value-based care models along with the increasing need to coordinate care, having a truly interoperable electronic health record is essential to modern practices. Certified EHR technologies (CEHRTs) are especially important in supporting value-based care, quality improvement programs, and ensuring seamless data exchange.
Tools like patient portals and advanced features like wearable technology further enhance the benefits of EHRs by enabling patients to take a more active role in managing their health. Understanding the differences and benefits of these digital health records is essential for healthcare professionals as they strive to provide the best care for their patients.
Is it time to trade your EMR for an EHR?
For healthcare providers who originally adopted an EMR to meet the 2014 requirement, it’s important to understand the benefits of switching to an EHR now. Having an EHR system can enable better care coordination across care sites and providers, drive efficiency through automation and record sharing, support providers interested in value-based care models, and ultimately improve patient outcomes. Additionally, a comprehensive solution that integrates the EHR with medical billing, revenue cycle management, and patient engagement capabilities, such as athenaOne, can increase efficiency across the entire patient encounter, from scheduling the appointment through care delivery all the way to billing and payment.
Read on to discover how an integrated EHR can provide levels of interoperability, efficiency, and coordination that simple EMRs cannot match. If you're ready to experience the athenaOne difference, explore the benefits now or schedule a meeting and get to know this all-in-one, integrated solution for medical practices and healthcare organizations of all sizes.
More electronic health record resources
Continue exploring
1. Based on athenahealth data as of Dec. 2024; M010
2. Based on athenahealth data as of Dec. 2024; M020