Top benefits of athenaIDX

Healthcare organizations today are facing unprecedented challenges. Shrinking reimbursements, difficulty collecting full payment, overwhelming administrative and operational burdens, increasing regulatory complexity, struggling to stay on top of industry changes, and high employee turnover rates pose serious threats to the long-term sustainability of healthcare organizations across the U.S. These issues can jeopardize access to care for millions of Americans, and according to a recent report, among the top five challenges for RCM teams in 2024 are timely patient collections (48%), managing denials (36%), and hiring and training staff (32%).1 It’s become increasingly difficult for healthcare organizations to stay afloat, with less than half (38%) of physicians stating they believe their organization is on solid financial footing.2
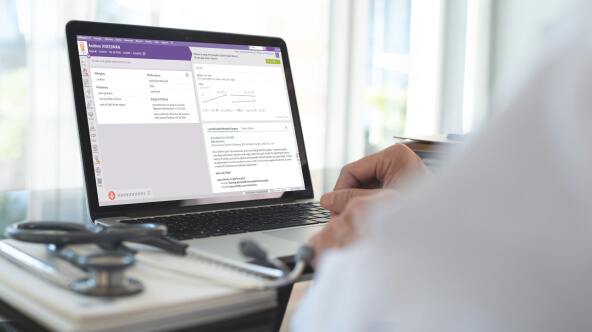
Understanding how to solve for these challenges is crucial for healthcare leaders if they seek to improve and sustain their organization’s financial performance. Using athenaIDX, hospitals, large organizations, and “payviders” can relieve administrative burden to focus time and resources on improving their bottom line. athenaIDX helps your organization transform the revenue cycle with you in the driver’s seat, helping you make data-driven decisions, reduce administrative burnout, increase staff productivity, and reduce overhead.
Below, we’ll dive into some of the ways that athenaIDX can benefit your healthcare organization by helping you optimize financial performance.
Transform the entire revenue cycle and increase collections with end-to-end RCM
Driving operational efficiency, employee productivity, and financial performance are top of mind for most large healthcare organizations today. But does your revenue cycle management software enable you to succeed, scale, and grow?
athenaIDX can help your healthcare organization optimize for efficiency and unblock payments across all stages of the revenue cycle:
- Front-end revenue cycle – athenaIDX helps FFS organizations benefit from patient estimation, quality registration, prepayments, financial assistance programs, rules-based, itinerary-driven scheduling, eligibility-specific copay/coinsurance/deductible collections at the point of service, and robust follow up care coordination. These key features help your organization to collect the right amount at the point of care, saving you time and money. For those organizations that are receivers of front-end data, your revenue cycle benefits from athenaIDX's inherent rules engine, ensuring complete registrations with Quality Assessments that surface missing, incomplete, inaccurate registration, insurance, eligibility, document, and enrollment requirements for clean billing downstream.
- Claim processing and scrubbing – athenaIDX automates tasks and segments work so that your staff can work by exception, helping make your revenue cycle low-touch. Intelligent charge capture and automation for correct coding, claim scrubbing and processing, and automated payment processing all help streamline the medical claims process for your organization. athenaIDX can help your organization achieve a 91% clean claim rate within the first 3 months of implementation.3
- Back-end revenue cycle –Using the same automation and work by exception strategies for bundled payment management, denial and underpayment resolution, A/R follow-up, and patient collections, athenaIDX can help your organization achieve A/R days as low as 26 days, helping your organization get reimbursed faster and more efficiently.4
Whether your organization is using a fee-for-service, value-based care, or hybrid payment model, athenaIDX helps organizations navigate them all, ensuring financial performance is optimized across the board in a variety of care settings and financial arrangements. Task management allows total control over every facet of accounts receivable, encompassing every payer, edit, and rejection. By providing actionable insights and auditing work at the most granular level, athenaIDX enables pinpoint identification and resolution of performance bottlenecks, helping to enhance A/R performance and minimizing collection costs.
To help you succeed with these new operations, athenaIDX implementation team members have an average of over 25 years of tenure and experience, helping you navigate complexities with a wealth of experience.
Automation tools help you optimize medical billing workflows and cut down on administrative tasks
Unlike other RCM software tools, athenaIDX uses low-touch, automated, rules-based workflows to help optimize operations, reduce collection costs, and expedite cash flow. athenaIDX has a unique embedded Transaction Editing System—a pre-A.R., intelligent charge capture solution—that can identify missing or inaccurate coding, and automatically update the charge transactions with accurate coding changes like adding/stripping modifiers, bundling or unbundling by payer rules, auto-swapping codes. Because these rules are controlled by your own compliance team, your organization can automate common coding corrections in real time, without manual intervention. Sophisticated contract management automatically evaluates payments for accuracy ensuring organizations collect what’s owed. Powerful in-app analytics provide real time insights into A/R activities and support strategic campaigns to increase collections and revenue capture across the board.
The athenaIDX EDI Clearinghouse helps enhance efficiency through integrated, concierge-managed workflows, achieving higher first-pass clean claim rates and improved point of service (POS) collections. With cleaner claims at the outset, your organization can help reduce denials, cut down on administrative work, and gain quicker reimbursement.
athenaIDX also helps ensure medical billing processes are effective and streamlined, working to minimize delays while maximizing revenue capture. Automation tools help free up staff resources so they can shift focus to more pressing challenges, reducing administrative burden along the way. The deployment of intelligent automation within athenaIDX also helps cultivate best practice workflows and paves the way for future operational efficiency and productivity within your organization.
Interoperability and enhanced data-sharing enable operational efficiency
Enabling healthcare providers and staff to obtain the right information at the right time is essential for any healthcare organization to run smoothly. Using athenaIDX, your organization can transform the revenue cycle while still maintaining a critical connection to all external care providers, enabling staff to coordinate care easily. Multi-entity management is also simplified with athenaIDX enterprise security affording you the ability to segment and secure your own markets with flexibility.
athenaIDX integrates easily with the leading EHRs and EMRs in the market, and features expansive modern interoperability, helping clinical staff make more informed decisions at the point of care and leading to increased patient satisfaction. Working in tandem with other external healthcare IT systems, athenaIDX helps break down information silos and ensures effective communication, collaboration, and data exchange across the healthcare continuum. athenaIDX provides comprehensive support for both RESTful APIs and SOAP services, enabling easy integration with a variety of customer service, patient engagement, payment, and EHR vendors, creating smooth and efficient data exchange allowing it to be the heartbeat of your organization.
This enhanced connectivity within athenaIDX revenue cycle software helps drive operational efficiency and provides a strong foundation for leveraging data analytics to drive informed decision-making and strategic planning.
Increased employee productivity*
To help your organization adhere to the new best practice workflows within athenaIDX, athenahealth Gamify works to drive staff engagement and productivity so employees can consistently hit their daily goals.
athenahealth Gamify is a staff-facing, game-like experience that sits on top of the athenaIDX RCM system and engages your medical billing team by allowing them to earn points for their performance and compete with fellow team members. Real-time data and actionable information allow you to keep organizational goals aligned, track individual performances with detailed analytics, and provide in-the-moment feedback that reinforces best practices. Celebrate your staff achievements with athenahealth Gamify and help reduce burnout by recognizing employee achievements and keeping them engaged.
*This is an add-on service not included with athenaIDX
By leveraging the power of athenaIDX, even for the most complex specialties, your healthcare organization can help increase patient payment collections, reduce collections costs, simplify processes and increase operational efficiency. Accelerating your organization’s revenue doesn’t need to be complex, and leveraging better tools and services can help cure complexity. Explore a better revenue cycle management solution with athenaIDX.
- Beckers Hospital Review, “The biggest challenges facing revenue cycle departments in 2024”, Jan 2024, https://www.beckershospitalreview.com/finance/the-biggest-challenges-facing-revenue-cycle-departments-in-2024.html
- 2023 Physician Sentiment Survey, commissioned by athenahealth and fielded by Harris Poll, Jan 2024
- athenaIDX Data as of December 2023 Note: The top quartile of athenaIDX ambulatory clients see a first claim payment success rate between 87.9% - 91.3% within the first 3 months.
- athenaIDX Data as of December 2023. Note: This metric is based off the top quartile of IDX ambulatory clients, which see AR days between 26.9 to 39.5 days in the first 3 months.