7 statistics about how athenaOne EHR beats the competition
Selecting which electronic health records system and practice management healthcare IT (HIT) software to use for your organization is a critical infrastructure decision that affects your daily workflow, ability to provide care to patients, and profitability. Since changing to new EHR software can be costly and cumbersome, physicians and practice managers know they need to choose wisely, thinking ahead for reporting and regulatory requirements as well as evolving technology and patient communication needs. You need an EHR system that meets you where you are now and grows with you as your practice and the healthcare regulatory and technological landscapes change.
Whether you’re a start-up practice choosing your first healthcare IT partner, a care center that digitized records early but now needs to upgrade their siloed EMR to an interoperable EHR system, or a physicians group that has outgrown the capabilities of their current electronic medical records software as they embrace value-based care contracts and alternate payment models, here are 7 data-backed reasons why athenaOne® may be the best EHR to choose as the backbone of your business.
1. Industry leading clean claim submission rate of 98.4%1
Let’s start off with a big one. Practices that use athenaOne have 98.4% of their claims accepted the first time they are submitted. That’s a better clean claims rate than any other system on the market. Pay attention when comparing stats on clean claims – many software vendors report claims that are submitted to payers, not claims that have been cleared for payment, or state that they aspire to a 98-99% clean claims rate. athenaOne actually achieves it.
Why does this matter? Cleaner claims mean you get paid faster, optimizing your cash flow so you can grow. It also means you have fewer administrative tasks and rework, allowing your practice to operate more efficiently. Your clean claims rate is one of the best predictors of your practice's overall revenue cycle efficiency.
When you’re an athenaOne client, you become part of an industry best revenue cycle management team and benefit from the insights of more than 160k providers2 on our network, helping you maintain a high clean claims average and an optimized revenue cycle.
2. Industry best claims rejection rate of only 1.6%3
This front-end rejection rate data point is the inverse of the clean claims rate, but it bears a closer look. Only 1.6% of claims submitted by athenaOne clients are rejected by payers before entering their adjudication system. athenaOne’s guardrails ensure that front-end staff capture important information about the provider, payer, and patient during the registration process, so claims won’t get kicked back to your practice to chase down necessary info, delaying your reimbursements.
The athenaOne EHR software has built-in checkpoints during the clinical workflow to walk staff through data entry of critical patient information, and the more than 30,0004 – and constantly updating – rules in our rules engine to scrub claims for missing, misaligned or inaccurate information before submission. All of these safeguards help ensure that your claims have what they need the first time, and athenaOne customers enjoy the lowest front end rejection rate in the industry.
3. >98% success rate in managing prior authorizations5
Prior authorizations are one of the greatest pain points physicians experience. On average, practices complete 43 prior authorizations per physician, per week.6 Plus, an overwhelming 95% of physicians report that prior authorization headaches contribute somewhat or significantly to physician burnout.7
Clients who rely on athenaOne and our team of authorization specialists have a 98% success rate for authorizations requested to get patients the care and prescriptions they need.8
Providers spend up to 16 hours a week on authorizations, and 35% of practices have a staff member who does nothing but deal with prior authorizations.9 Get that time back by letting athenahealth complete authorizations on your behalf, and let clinicians spend more time with patients.
Our dedicated authorization specialists begin work on an urgent authorization task in under 2 hours and in less than 24 hours for non-urgent PA requests. And our team gets it done: less than 2% of authorization requests to payers end in a negative outcome when our authorization specialists work the orders.10
Clients who work with athenahealth for prior authorizations not only get faster results and save themselves time, but they have a superior success rate for their patients getting the care you order for them and that they need.
"When you’re an athenaOne client, you become part of an industry best revenue cycle management team and benefit from the insights of more than 160k providers on our network."
4. 48% higher patient pay yield11
Wouldn’t you like to collect more of the patient balances you are owed for services provided? Practices that use athenahealth’s online patient payment solution have a 48% higher Patient Pay Yield (PPY) than practices that do not. PPY refers to the percentage of a patient balance that is collected within six months of the date of service.
Using athenaOne’s convenient patient billing reminders, easy patient payment interfaces, and integrated online payments, our clients collect 48% more of outstanding patient balances than non-athenahealth customers, on average.
Collect more of what you’re owed by using the user-friendly payment tools integrated in athenaOne and earn strong patient satisfaction ratings by making the process of payment easier, more transparent, and more convenient.
5. Get paid 15% faster with athenaOne’s online patient payments
athenaOne clients using the online patient payment solutions get paid nearly 50% more of the patient balances they are owed, and they also get paid 15% faster, for an optimized revenue cycle and steadier cashflow.12
athenaOne has built-in, customizable dashboards that calculate a practice's rolling Days in Accounts Receivable (DAR), among other metrics, so you can track how long it takes to get paid. Practices that use athenaOne’s online patient payment capability streamline their patient payment cycles and offer convenience to patients to pay easily and securely online, for a win-win for the patient and the practice.
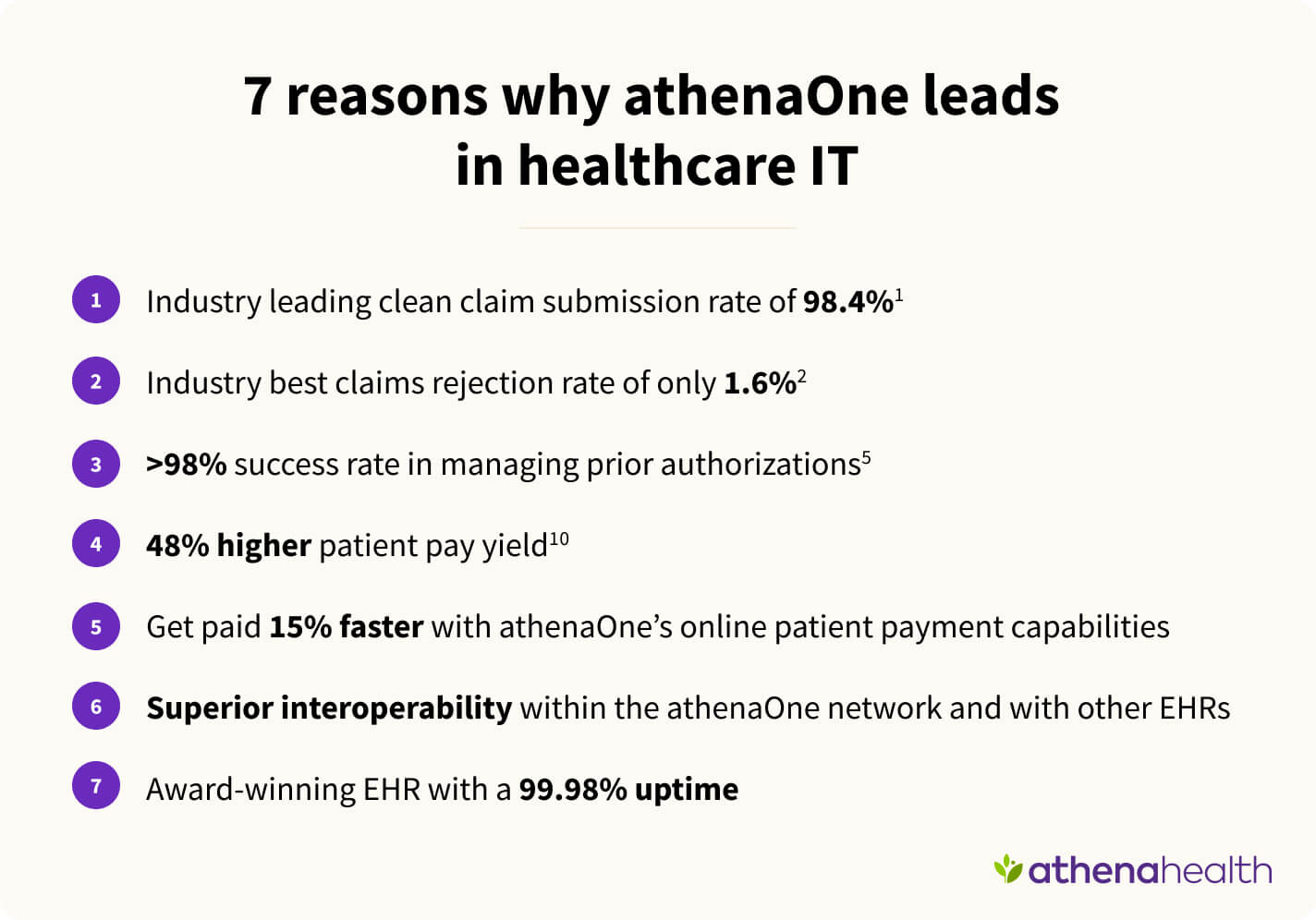
6. Superior interoperability within the athenaOne network and other EHRs
As we work to implement coordinated care through record sharing across hospitals, labs, doctors, payers, and clinics, interoperability – or the ability to exchange patient data securely and efficiently – is ever more important, especially for value-based care models and CMS healthcare regulations requirements.
athenaOne customers have access to 165K+ clinical integrations (total connections to labs, imaging centers, pharmacies, patient record sharing networks, health information exchanges and registries).13 Some, such as patient record sharing, are immediately implemented, and others are available for integration depending on your practice’s needs.14
Keep track of your patients as they visit other specialists or have a hospital stay. athenaOne’s electronic health record software has automatic connections to 100% of health systems using Epic and 66% of Cerner electronic health records who participate in Carequality and CommonWell for data exchange.15
What does that mean for doctors? It’s easier to exchange information with other medical providers using athenaOne, leading you to more efficient clinical workflows and more holistic knowledge of a patient’s diagnoses and overall health, helping you make better decisions at the point of care and improve their health outcomes.
7. Award-winning EHR with a 99.98% uptime
You might think that stable and secure access to your EHR or practice management system would be table stakes, but not all HIT software solutions are created equal. Vendor service disruptions can be costly to healthcare organizations – leading to patient dissatisfaction, lost efficiency, and even lost revenue. That’s why athenaOne has reduced our service disruptions to 0.02%.16
Our cloud-based EHR, PM, RCM, and patient engagement software has an industry leading 99.98% uptime17, so athenaOne is there when you need it, a stable and reliable HIT solution, no matter what time of day or night you are accessing it.
As a Certified Electronic Health Records system, athenaOne is also fully compliant with HIPAA requirements for patient privacy and data security. Our industry-leading uptime means athenahealth is a trusted software partner for your practice.
In fact, athenaOne was named Best in KLAS 2024 for Small Practice, Ambulatory EHR/PM, Independent (2-10 Physicians) and for Ambulatory EHR, Independent (11-75 Physicians). Benefit from the extraordinary security, reliability, and usability of athenaOne and see why it is recognized by KLAS year over year and trusted by over 160,000 medical professionals in the United States.
Learn more about athenaOne and see for yourself
If these industry-leading data points have piqued your interest, book a call with a member of our sales staff to see athenaOne in action and learn how we can support you in making the switch to a next generation integrated electronic health record, practice and revenue cycle management, and patient engagement HIT solution that puts the power of the nation’s largest provider network to work for you and your practice.
- Based on athenahealth data for twelve months ending Mar. 2024; results compared to competitors' self-reporting of clean claim submission rates; M164
- Based on athenahealth data for twelve months ending Mar. 2024; results compared to competitors' self-reporting of front end rejection rates; M169
- Based on athenahealth data as of Sept. 2024; M010
- Based on athenahealth data as of Mar. 2024; M017
- Based on athenahealth data as of Dec. 2023; M161
- AMA, Dec. 2023, 2023 AMA Prior Authorization Physician Survey, pg.2;https://www.ama-assn.org/system/files/prior-authorization-survey.pdf; IS059
- AMA, Dec. 2023, 2023 AMA Prior Authorization Physician Survey, pg.2;https://www.ama-assn.org/system/files/prior-authorization-survey.pdf
- Based on athenahealth data as of Dec. 2023; M161
- AMA, Dec. 2023, 2023 AMA Prior Authorization Physician Survey, pg.2;https://www.ama-assn.org/system/files/prior-authorization-survey.pdf; IS057
- Based on athenahealth data as of Dec. 2023; M161
- Based on athenahealth data as of Jun 2024. Patient Pay Yield (PPY) is the percentage of patient balance collected within 6 months of the date of service; M046
- Based on athenahealth data as of Dec. 2023; compares the number of days it takes practices to get paid with or without the use of athenahealth's online payment solutions; M047
- Based on athenahealth data as of Dec. 2023; M020
- Based on athenahealth data as of Dec. 2023; M020
- Based on CommonWell and Carequality data as of Jun 2024; M025
- Based on athenahealth data for twelve months ending Jun. 2024; M019
- Based on athenahealth data for twelve months ending Jun. 2024; M019