Resource Center
All ContentBlogCase Studies
- athenahealth
- March 11, 2025
- 9 min read
10 ways patient engagement tools enhance healthcare
From scheduling to billing and care coordination, these patient engagement tools help patients and practices thrive. Read moreYou may also like

- Christine Davis
- April 02, 2025
- 5 min read
athenahealth products
An EHR built for behavioral health
Behavioral health providers need technology that supports their unique needs. See how we deliver.
Read more 
- athenahealth
- April 02, 2025
- 7 min read
Electronic health record
The hidden costs of an unreliable EHR
When your EHR doesn’t live up to its promise, it can end up costing you more. Explore what to look for in a reliable system.
Read more 
- Christine Davis
- April 02, 2025
- 8 min read
athenahealth products
athenaOne® features that reduce patient charting time
See how EHR tools, accelerators, and Ambient Notes are helping clinicians document faster.
Read more 
- athenahealth
- April 02, 2025
- 8 min read
Shared savings VBC
Guide to Medicare accountable care organization models
Do you understand CMS' ACO payment models? Read our guide to find programs for your practice.
Read more 
- Christine Davis
- April 02, 2025
- 5 min read
athenahealth products
An EHR built for behavioral health
Behavioral health providers need technology that supports their unique needs. See how we deliver.
Read more 
- athenahealth
- April 02, 2025
- 7 min read
Electronic health record
The hidden costs of an unreliable EHR
When your EHR doesn’t live up to its promise, it can end up costing you more. Explore what to look for in a reliable system.
Read more 
- Christine Davis
- April 02, 2025
- 8 min read
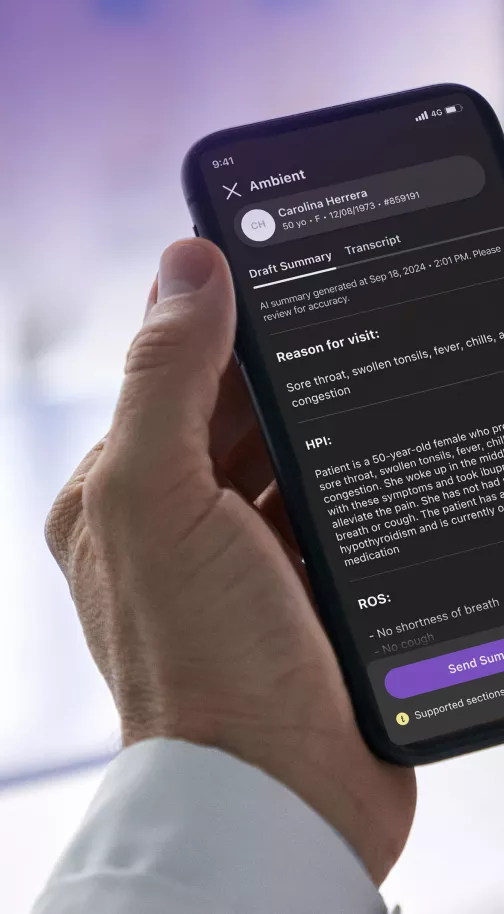
athenahealth products
athenaOne® features that reduce patient charting time
See how EHR tools, accelerators, and Ambient Notes are helping clinicians document faster.
Read more 
- athenahealth
- April 02, 2025
- 8 min read
Shared savings VBC
Guide to Medicare accountable care organization models
Do you understand CMS' ACO payment models? Read our guide to find programs for your practice.
Read more 
- Christine Davis
- April 02, 2025
- 5 min read
athenahealth products
An EHR built for behavioral health
Behavioral health providers need technology that supports their unique needs. See how we deliver.
Read more Empower your practice

AI powered patient engagement
Learn how AI tools can help improve patient loyalty and outcomes.