Across the athenahealth network and beyond, healthcare organizations are designing and implementing simple interventions with outsized impact on outcomes, satisfaction, and success. Here's another.
The problem
Often patients with behavioral health challenges don't realize they have a condition, resist treatment because of the stigma, or can't pay the higher specialist copay to see a psychiatrist.
Providers at Queen's Clinically Integrated Physician Network (QCIPN), a 1,100-physician network in Hawaii, continually identified behavioral health as a key concern in managing their high-risk, high-need patients.
However, the national shortage of psychiatrists, low statewide reimbursement rates, and the highest cost of living in the nation make finding a psychiatrist for a patient in Hawaii particularly difficult – especially if the patient is on Medicare or Medicaid.
The solution
In 2016, QCIPN piloted a collaborative care program (initially developed at the University of Washington AIMS Center) to extend the reach of available psychiatrists and integrate behavioral health into primary care. In this model, social workers become care coordinators, helping patients who aren't comfortable seeing a behavioral health professional on their own, or whose insurance would not cover a specialist visit.
The first step is to use standard behavioral health screenings with all patients, not just those perceived to be at risk. Those who have mild to moderate depression, and are unwilling or unable to make a one-on-one appointment with a psychiatrist, are candidates for enrollment in the collaborative care program. Each is then assigned to a social worker who acts as care coordinator.
The care coordinator reviews the patient's medical record and confers with their primary care physician, so coordinators are fully informed before they contact the patient.
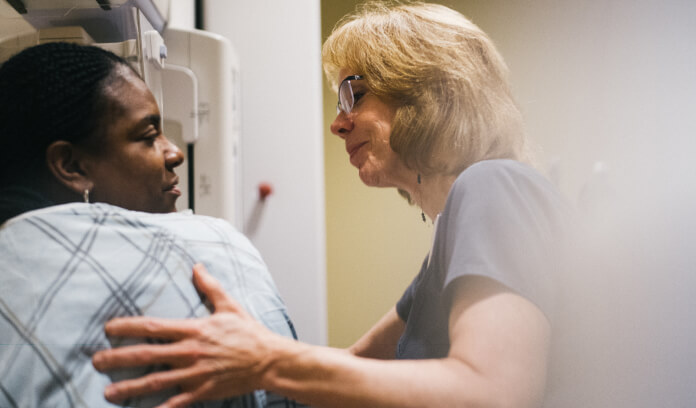
Coordinators then set up an initial hour-long meeting, in-person or by phone, with the patient to set expectations and gain understanding of the patient's condition, concerns, and personal health goals. Next the coordinator presents the case to one of two on-staff collaborative care psychiatrists to determine a care plan.
I'm still going to be the quarterback, but we collectively are going to manage your care.
The PCP signs off on the plan and orders any medications. “The PCP is still the nucleus of the care team," says Mia Taylor, manager of clinical programs at QCIPN. “That's the really important piece. The PCP is saying, 'I'm still going to be the quarterback, but I am asking for additional help from my colleagues, and we collectively are going to manage your care.'"
The coordinator facilitates referrals to psychotherapy if needed, and calls the patient weekly to check in and answer any questions. If the patient has comorbidities, the coordinator will consult with a nurse so they can collaboratively manage all the patient's care, scheduling an in- person appointment when necessary. And the whole team reviews cases once a week and manages care going forward.
Overall, the collaborative care model provides far more frequent touchpoints than the traditional models of mental health or primary care, all through the PCP's office. And early indications are that the extra cost of staff is offset by better health outcomes and reduced hospitalizations and emergency visits.
The outcome
QCIPN is tracking data around remission of disease, total cost of care, 30-day readmissions, emergency department visits, hemoglobin A1c levels, and blood pressure. Initial analysis shows significant improvements through the collaborative care model, Taylor says. “We are hopeful to be able to see improvement in all measures. I'm convinced that we're going to be able to show ROI."
At QCIPN, 95 percent of patients referred to the program are actively engaging in treatment. Compare that to the national average, in which only 50 percent of patients referred for mental health care actually follow through. Taylor believes that increased screening – the first step in the collaborative care model – may be catching as many as 70 percent more patients who have anxiety and depression.
And PCPs say they are better physicians now that they're more actively looking for behavioral health issues and having the resources to support patients with these needs. As one PCP with a particularly complex panel of patients noted, “There's no way I could have managed these patients without the help of collaborative care and my home-based team."
Lia Novotny is a contributing writer to athenaInsight.