Assessing your readiness for Alternative Payment Models
If you're an experienced healthcare professional, you know value-based care (VBC) can be complex. If you're new to VBC, knowing if and when you're ready to start taking advantage of the many Alternate Payment Models (APM) available to healthcare organizations today can be a challenge.
For other information on VBC, including an overview of APMs, you can find a selection of articles here.
What follows is a structured approach to help you think through and decide if you're prepared to leverage value based medical care and the variety of healthcare payment models it includes, along with some practical actions to take today if you're not there yet.
Ready to start? Considering the following questions:
1. Do you understand the value based care model options available to you?
The primary reimbursement models available under VBC can be bucketed into three primary categories: pay for performance (P4P) or bundled payments; shared savings programs; and capitated or upfront payments.
Pay for performance or bundle payments
Pay for performance (P4P) or bundled payments reward providers for meeting certain quality-related requirements and metrics, like general patient satisfaction or improvements around certain measures for chronic conditions like diabetes, hypertension, and others.
P4P financial incentives are typically distributed as either upward or downward adjustments to your Medicare Part B fee schedule. For example, CMS’ Merit-based Incentive Payment System (MIPS) is an example of P4P.1
Shared savings programs
Shared savings programs encourage medical practices to form Accountable Care Organizations (ACOs) to deliver comprehensive, high-quality care to specific groups of patients while limiting or avoiding unnecessary (or duplicative) costly services and interventions.
Generally, shared savings programs encourage collaboration among healthcare entities to find efficiencies and lower costs; participating practices are then eligible to receive a portion of the savings. CMS’s Medicare Shared Savings Program (MSSP) is an example of shared savings.2
Capitated or upfront payments
Global capitation programs incentivize healthcare organizations to take on financial risk associated with high-risk patient populations. Incentive payments are distributed upfront, or before care is delivered, which is one of the primary benefits of capitation in healthcare. Participating practices that keep costs below these monthly payments can keep the surplus.
Medicare’s Program of All-Inclusive Care for the Elderly (PACE) is an example of a capitated program.3
2. What are the characteristics and demographics that make my practice unique?
Every medical practice is unique. Every physician has special knowledge and experiences that have formed their approach to care. Your patients also bring with them a unique and ever-evolving set of needs. Understanding these characteristics is the first step toward selecting the right VBC program.
For example, what are the demographics, health needs, and payer mix of your patient population? Does it include many high-risk, high-cost patients? Do you have opportunities to offer sustained preventive care or chronic disease management? What percentage of your patients receive benefits through Medicare?
The answers to these types of questions should provide direction for which APMs are well-suited for your needs as well as your patients. A consolidated healthcare IT (HIT) platform with integrated population health analytics should enable you to analyze and report on this information as needed.
3. What level of support do you have from your healthcare IT vendor for VBC and risk management?
Levels of financial risk are an important consideration in the design of APMs. Some programs carry little financial risk; though the incentives are lower, these programs can be right for smaller, independent practices with limited resources. Other programs are designed for healthcare organizations that are large and complex enough to take on financial risks (and potential rewards) without threatening the health of their business.
If you’re new to VBC, managing your risk and revenue streams from APMs can feel both complex and unpredictable. And for good reason—many practices getting started with VBC are not adequately prepared to manage the associated risk, which can lead to financial instability and a reluctance to fully embrace value-based care initiatives.
However, the right healthcare IT partner can help you overcome these hurdles. The right partner can deliver both the expertise and services you need to round out your capabilities. Actively analyzing your data, providing detailed and clear documentation, proactively communicating program milestones and requirements, developing timely software updates to comply with changing regulations, and providing resources on emerging best practices are all areas your HIT partner should help bridge the gap.
If you’re feeling overwhelmed by the complexity of VBC, that’s normal. With the right support, that complexity doesn't have to prevent you from taking on more risk and achieving more incentives.
4. Do you have access to your practice's historical data?
Part of determining which APMs to consider is understanding the big picture of the work you and your colleagues do on a year-to-year basis. Getting this high-level view of both your clinical activity and financial performance over time can help you see where your current strengths are, and where you should focus future growth.
For example, do your current medical billing tools and processes enable you to view and report on historic claims data? If so, are you able to use that historical claims data to simulate performance under the models you are considering? This type of data fuels predictive analytics that can help you find the right balance of programs with less trial-and-error.
Historical data can also give you a more nuanced view of your current state costs, provide views into your performance in achieving certain quality metrics, and help you identify where you best opportunities for cost savings are going forward.
5. Are your practice's standard operations flexible enough to support APM participation?
How well does your team adapt to change? Are the core processes and tools you have in place today adaptable as well? Value-based care is intended to address some of the fundamental inefficiencies in our healthcare system, so some degree of operational change will be necessary to accommodate this new approach, whichever programs you select.
Two places to start are staff training and workflow adjustments. Do you have an ongoing training program for staff? A regular training cadence can help everyone get used to the idea of change and begin laying the groundwork to do so effectively.
What about your electronic health records (EHR) system? Does it support value-based care? Will it allow you to tailor your workflows to make the most of these programs?
6. Have you involved your key stakeholders in your decision process?
Building consensus around your move into value-based care is vital to your success with any new APM. And as with any significant change, it can be easy to get consumed with the details and forget to make sure your fellow travelers are informed and as bought-in as you are.
If you’re a practice manager or physician at a larger organization, be sure to involve as much of the clinical and support staff as possible. Remember, VBC involves much more than face-to-face time between physicians and patients—it requires buy-in from everyone, from front desk staff to medical billers.
Moving into value-based care is also a great opportunity to remind your patients that you have their best interests in mind, and that you’re actively working to improve care and bring down costs. Your patient engagement solution should enable you to push out communications to let your patients know what you’re up to; that same solution will be useful if the program you choose includes quality metrics around adherence to care plans.
7. Who are the industry participants that can provide guidance?
As you dig deeper into various APMs and VBC generally, expect to have questions. A whole industry is working to shift these paradigms of US healthcare.
Thankfully, you shouldn’t have to navigate these changes alone. What kind of support do you have access to in your area? Do you have relationships with other providers in the region that are at a similar or more advanced stage in their journey to VBC? Engage with those peers and ask what lessons they’ve learned so far.
There are also industry consultants who can help. For instance, your healthcare IT stack may include vendors with deep expertise in value-based care. They’ve likely helped many practices similar to yours navigate similar questions and challenges.
Also be sure to look into the Centers for Medicare & Medicaid Services’ (CMS) Quality Improvement Organization (QIO) program.4 Your regional CIO’s mission is to improve health care quality, access, value and equity for people with Medicare and is there to support you and your patients.
8. Can you run a pilot to test an APM program?
If you’re not quite ready to incorporate your first APM program today, there are steps you can take to help get you there. One example is running a pilot program to test the effectiveness of, and your readiness for, the program you’re considering.
There are formal and informal ways to do this. For example, the CMS is running the Making Care Primary (MCP) model designed as a “pathway for primary care clinicians with varying levels of experience in value-based care to gradually adopt prospective, population-based payments while building infrastructure to improve behavioral health and specialty integration and drive equitable access to care.”5 Designed with three progressing tracks, the program provides funding and support for qualifying primary care providers to build their VBC capabilities. The program is currently being tested in eight states.
If you don’t qualify for MCP, consider designing your own pilot program by identifying and tracking specific quality metrics and calculating your performance over time. From there you can evaluate outcomes and expand involvement in more advanced models based on success.
9. Do you have the capabilities to monitor and reassess your participation?
Monitoring your performance in the APM programs you choose should be done on an ongoing basis. You should be able to regularly review performance and patient outcomes data against program goals and thresholds to see how well you’re doing.
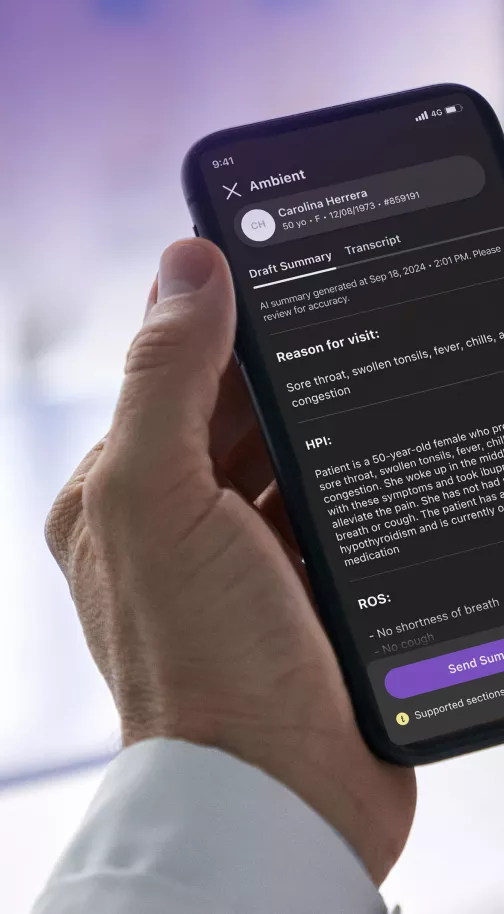
Using a capable EHR with real-time reporting capabilities is the best way to achieve this. You should be able to see your up-to-date performance in real time so you have the info you need to make adjustments as you go. An innovative platform like athenaOne can add further value by proactively assessing your data so you can report the most optimal performance data for your programs. Lacking these capabilities should be a red flag that your EHR isn’t doing enough.
This reporting can also help boost your performance in other ways: for instance, it may help identify additional care gaps you can close, a key quality metric in many programs.
10. Do you have long-term goals you’re working toward?
What are your long-term goals for your practice? Do you want to be independent, or do you hope to join a health system? Do you want to expand to new services, offices, or regions? Are you part of an ACO, or hoping to form one? These are important strategic factors; consider how the various APM programs you’re evaluative can help you get there.
Start by aligning an APM with your practice’s mission, vision, and sustainability objectives. Are they complimentary? Also ensure that your chosen model supports both financial health and improved care delivery.
Again, a HIT partner with VBC expertise and a broad view of the industry can help you understand how various programs can fuel your strategic direction.
By carefully weighing these factors, you may be able to identify an APM that aligns with your capabilities and goals while minimizing risks.
Now you know where you stand. What next?
Now that you’ve considered your readiness for VBC from a variety of angles, where do you stand? It’s likely you already have some or many of the capabilities you’ll need to participate and succeed in a number of VBC programs.
Regardless of which programs you’re interested in, focus on these core competencies:
Understand your patient population:
Invest in technology that provides a detailed and ongoing view of the patients you serve. Understanding your patients’ levels of risk, payer arrangements, and analytics on the common services you provide will help you build this knowledge.
Invest in interoperability:
Care coordination is a top-line goal of value-based care. Success in VBC depends on true interoperability. In fact, certain programs require you to use EHR technology that is certified by CMS and the Office for the National Coordination for Health Information Technology (ONC).6 Is your technology ONC-certified? More important: does your EHR surface the actionable clinical data it aggregates when and where you need it? It should.
Find an industry partner like athenahealth who has the expertise, technology, and servicing capabilities to help you start your VBC journey and succeed with the programs you select.
Ask for help
Getting started with Alternative Payment Models may feel overwhelming to you now, but don’t give up. Find an industry partner like athenahealth who has the expertise, technology, and servicing capabilities to help you start your VBC journey and succeed with the programs you select.
athenaOne for Alternative Payment Models
No matter where you are in your value-based care journey, athenaOne can help you take your next step toward prioritizing quality and achieving the great incentives available to you through value-based care. Our integrated platform combines software and services for electronic health records, practice and revenue cycle management, and patient engagement. Further innovations, like the Patient Digital Engagement Index, payer integrations, and purpose-built reporting for specific quality-based programs, add additional value.
Teams of experts—including a dedicated customer success manager—help you make the most of athenaOne, and also help you understand the ins and outs of quality-based programs, how your peers are leveraging them, and how to find the operational efficiencies you need to enroll in value-based care programs that will benefit you and your patients alike.
For more information, read the articles below or visit our selection of value-based care information, Value-based care, explained.
1. CMS, Traditional MIPS Overview; https://qpp.cms.gov/mips/traditional-mips
2. CMS, Jan. 2025, Shared Savings Program; https://www.cms.gov/medicare/payment/fee-for-service-providers/shared-savings-program-ssp-acos
3. CMS, Jan. 2025, Program of All-Inclusive Care for the Elderly; https://www.cms.gov/medicare/payment/fee-for-service-providers/shared-savings-program-ssp-acos
4. CMS, Sept. 2024, Quality Improvement Organizations; https://www.cms.gov/medicare/quality/quality-improvement-organizations
5. CMS, Making Care Primary (MCP) Model; https://www.cms.gov/priorities/innovation/innovation-models/making-care-primary
6. CMS, Sept. 2024, Certified EHR Technology; https://www.cms.gov/medicare/regulations-guidance/promoting-interoperability-programs/certified-ehr-technology