The power of the network: How athenaOne® benefits physicians
Clinicians need more than just an electronic health record platform that can meet regulatory requirements and basic operational needs. What today’s clinicians and practices need is an integrated EHR, patient engagement, and revenue cycle management and billing solution system that works for them, not against them.
Many EHRs and practice management software operate in isolation, making it difficult to benchmark performance, streamline workflows, and coordinate patient care. athenaOne’s single-instance SaaS (Software as a Service) model eliminates these barriers by connecting 160,000+ clinicians1 on a unified cloud-based platform, delivering real-time insights, efficient interoperability, and automated optimizations. Whether you’re a solo practitioner or managing a multi-site medical group, the power of the athenahealth® network helps you maximize revenue, improve patient outcomes, and reduce administrative burden, without the IT headaches of traditional EHRs you’ve come to know – and dislike.
Why a single-instance SaaS EHR makes a difference
Unlike traditional on-premise or siloed EHR systems, athenaOne operates as a true SaaS cloud-based platform, meaning all 160,000+ clinicians are on the same instance of the software no matter when they started using athenaOne or where they are located. It also means that all practices on the network always have the newest version of the software: software updates are made at scale.
This unified network enables real-time data analysis, benchmarking, and actionable insights across a vast ecosystem of providers. The power of the network enhances the athenaOne suite of software and services, adding valuable benefits that can’t be found in siloed software installations, even from the cloud.
Here are some key benefits for physicians, clinical staff, and medical practice managers gained when you join the largest connected healthcare network in the United States as an athenaOne user:
1. Smarter clinical & operational insights from a nationwide network
Because athenaOne aggregates deidentified data from every provider on the platform, physicians can benefit from:
- Real-time benchmarks – Compare key performance indicators (KPIs) like patient outcomes, billing efficiency, and practice revenue against practices of similar size, specialty, and location. This can help you learn from others to improve your practice’s coding, revenue, and patient outcomes.
- Evidence-based best practices – Access data-backed treatment trends, helping physicians choose the most effective interventions based on real-world outcomes. Are more doctors prescribing a different medication to treat a common illness than you are, for example? Or perhaps other clinicians are ordering an additional type of test when they see a specific set of symptoms among patients. You’ll be able to see common actions and relevant information to help hone your clinical decision making.
- Local & regional insights – Understand disease prevalence, treatment success rates, and payer trends specific to your community, and across wider geographic areas, including nationwide. This can be especially relevant with infectious diseases such as RSV and the flu, or help with chronic care such as obesity, heart disease, or diabetes.
- Discussion with other clinicians and providers – The athenahealth network includes over 44,000 active participants in the athenaOne Customer Success community,2 as well as 56 user groups.3 Physicians and medical staff can join different free online user groups to share best practices, learn new strategies, and collaborate with peers, fostering a culture of continuous improvement and support.
Here’s how leveraging evidence-based best practices can work. Imagine a primary care physician in a metropolitan area who sees that local peers have higher reimbursement rates for annual wellness visits. This insight helps them adjust their coding practices to capture full reimbursement and stop leaving provided billable services unclaimed. From relevant discussion that is the pulse of emerging trends in American healthcare to practical how-tos and tips for efficient use of athenaOne, athenahealth’s insights dashboards and success community bring the power of the largest network in healthcare to your fingertips.
2. Continuous improvements without IT headaches
With a single-instance SaaS model, athenaOne updates automatically for all users, eliminating the need for expensive IT maintenance or upgrades.
- Updates without interruptions – New features, compliance updates, and security patches are applied automatically, without having to go offline.
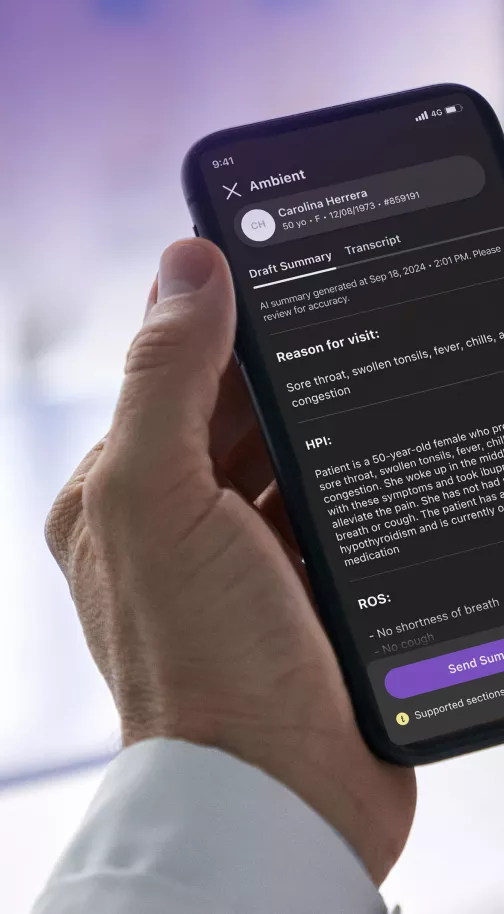
- Always the latest technology – Physicians benefit from AI-powered workflows, improved user interfaces, and new integrations without extra costs. You never need to worry about being on a previous version that becomes unsupported or having to do the cost-benefit analysis of paying for an upgrade.
- Zero infrastructure costs – No need for on-site servers, IT teams, or manual software updates. Whenever you log on, you’ll know you’re on the latest version, no matter the device or clinic location. All that’s required is a computer, tablet, or mobile phone with internet access – something you have for your practice’s daily operations.
For example, when new CMS billing codes are introduced quarterly or annually, athenaOne updates across the network instantly, preventing claims denials that would otherwise result from outdated codes. athenaOne also is updated three times per year with new features and enhancements – many of which are suggested by our users through our Voice of the Customer program. In 2024, we implemented more than 360 customer ideas in our products, accounting for 38% of the product enhancements we made that year.4 Everyone benefits from these automatic upgrades that introduce new templates, text macros, AI-enabled features, and other accelerators to streamline workflows, reduce clicks, and close encounters faster and with less effort.
By joining the athenaOne network, physicians gain access to a powerful, data-driven ecosystem that continuously evolves to meet the needs of modern healthcare.
3. Faster, more accurate claims processing & revenue optimization
Because athenaOne processes millions of claims across nearly every medical specialty and size of practice, the power of the nationwide network can detect patterns in denials and reimbursements and surface them to help physicians optimize their revenue cycle.
- AI-driven automated claims scrubbing – More than 29,000 constantly updating rules and algorithms5 help identify billing errors before submission, reducing denials and improving cash flow.
- Payer-specific trends – athenaOne automatically has integrations with many of the largest healthcare payers in the United States – right in the EHR and surfaced at the point of care. These insights help clinicians learn which insurers deny certain claims most frequently, allowing practices to adjust clinical documentation before submitting claims and to help them let patients know the cost of care and available alternatives in real time.
- Benchmarking reimbursement rates – Compare your practice’s reimbursement rates against peers in the same specialty, region, or practice size. Having this data at your fingertips can help you evaluate your fee schedules and coding practices to learn if you are leaving money on the table for services you provided or additional best practice services that could close care gaps and improve revenue.
As an example, using the athenaOne insights dashboard trained on data from over 315 million annual claims6 and 72 million patients7 nationwide, Tarpon Interventional Pain and Spine Care has been able to benchmark its financial performance against that of its peers on the network, and adjust accordingly. “We can easily see whether we are being paid accurately,” says Chief Financial Officer Dede Arnold. “Are we underpaid or overpaid? Are we getting reimbursed to cover our costs? Things like that were impossible to see before athenaOne.”
4. Population health & predictive analytics for better care
athenaOne’s network analyzes deidentified data across its 160,000+ clinicians to identify trends in chronic diseases, medication adherence, patient communications, and preventive care gaps.
- Early identification of at-risk patients – AI-powered alerts flag patients likely to develop chronic conditions based on similar population data from across the network. This can help you determine a diagnosis sooner and start managing it with a healthcare plan more quickly or allow you and the patient to take action that may stave off the chronic condition longer with effective interventions and changes.
- Improved care coordination – Insights help primary care providers, for example, see how their patients’ specialty and hospital visits impact their health outcomes, while specialists and hospitals can review PCP notes for more informed and holistic care.
- Better preventive care programs – Physicians can proactively intervene based on data showing which patients need follow-ups. Data insights from the network help predict which actions have the greatest impact for improving care and maintaining wellness.
As an example of this benefit in action, a doctor may learn that patients with a certain comorbidity profile have a higher risk of hospital readmission within 30 days. This insight can prompt the doctor to follow up sooner, potentially reducing hospitalizations.
5. A true network effect for referrals & interoperability
Unlike EMRs and EHRs that operate in server-based silos, athenaOne enables efficient referrals to other athenahealth providers and interoperability across its network, right from day one.
- Easier referral management – Physicians can refer patients within the athenaOne network and instantly share clinical data, lab results, and imaging – directly into the EHR, not as a PDF attachment several clicks away.
- Reduced administrative burden – No need for faxing, manual data entry, or chasing records from outside providers. athenaOne’s data normalization efforts and ChartSync features help automate, interpret and display exchanged data where and when you need it.
- Better care transitions – Specialists and PCPs quickly and efficiently share data, leading to faster diagnoses and treatment adjustments. When you update a patient’s record or lab results come in, all care team members have easy and updated access for unmatched care coordination.
Allegro Family Clinics of Mississippi has tapped into the power of the network to reduce their administrative burden around prior authorizations. Instead of spending 30 to 45 minutes chasing each authorization needed, Allegro now uses athenaOne® Authorization Management to handle the process on their behalf, whittling the time spent to just two minutes in many cases.* The service automatically checks the order against payer requirements to determine if an authorization is required; if so, athenahealth’s authorization team handles the submission and follows up with the payer.
6. Adaptability to different practice sizes & specialties
One of athenaOne’s greatest strengths is its ability to scale and provide relevant insights based on the unique needs of small, mid-sized, and large practices. Whether you’re a solo practitioner aiming to maximize efficiency or a multi-site healthcare group looking for enterprise-wide optimization, athenaOne delivers tailored benefits for your practice size, type, and specialty.
Small practices (1-5 clinicians)
Small practices often operate with limited administrative staff, meaning efficiency and automation are critical to success. athenaOne helps these practices by:
- Automating billing & claims management – A single-physician practice can benefit from AI-powered claims scrubbing, which is informed by insights from denied claims across the 160,000+ clinicians on the network. This helps to ensure fewer denials and faster reimbursements without needing a dedicated billing team. Fewer hours spent on admin tasks means more time and attention to patient care.
- Benchmarking against similar practices – A physician-owned family medicine clinic can compare their coding and revenue cycle management with similar-sized practices, identifying missed revenue opportunities that help keep this partnership independent.
- Reducing administrative burden – Instead of being overwhelmed by time-consuming tasks such as manual data entry or chasing down patient records, a small dermatology practice with limited staff can benefit from athenaOne’s automated workflows informed by the performance of other dermatologists across the network. This can help streamline patient intake, documentation, and follow-ups, freeing up time for patient care.
Dr. Lianna Lawson opted for athenaOne’s extended revenue cycle management services when the burden of handling medical billing and coding tasks in-house became too great. Soon after upgrading to athenaOne Medical Coding, Enhanced Claim Resolution, and Authorization Management, she found that she had previously been missing out on $50,000 per year in reimbursements.* Now, her four-clinician family practice can bill quickly and comprehensively, realizing additional revenue.
Mid-sized practices (6-19 clinicians)
Growing practices with multiple specialties or locations need tools that help standardize workflows, improve financial performance, and manage patient volume. athenaOne supports these needs by:
- Multi-location analytics – A cardiology group with 10 providers across three locations can use centralized data to track patient volumes, appointment no-shows, and reimbursement rates across all sites.
- Guiding strategic growth – A mid-sized orthopedic practice or urgent care center looking to expand can analyze which services are most profitable and assess patient demand trends before opening a new office or clinic location.
- Improving staff productivity – A 12-provider pediatric practice can leverage AI-driven scheduling insights from their own and similar practices on the network to ensure optimal clinician coverage, reducing patient wait times and maximizing appointment slots.
After wrestling with a labor-intensive manual patient payment tool, TrustCare Health leveraged athenaOne and marketplace partner Rivia Health to automate their patient billing process end to end. Rivia Health’s touchless payment engagement solution notifies patients about outstanding balances via text and allows the patient to pay in full or set up a payment plan. It doesn’t require staff input or manual entry, and its pre-existing integration with athenahealth enables data to flow bi-directionally to and from Rivia Health to athenaOne, instantaneously. According to TrustCare, this saves them about 389 hours a month on operational tasks.*
Large practices (20+ clinicians, multiple locations)
Enterprise-level medical groups require robust data-sharing, system-wide standardization, and advanced operational insights to ensure smooth and scalable care delivery. athenaOne excels in:
- Enterprise-wide data integration – A multi-specialty group with 50+ clinicians can efficiently share patient records, lab results, and visit notes across locations, ensuring continuity of care.
- AI-driven staffing & scheduling – A large urgent care chain can use predictive analytics to optimize provider schedules, balancing patient demand with staff availability across multiple clinics.
- Consistent quality metrics across locations – A hospital-affiliated primary care network can track provider performance, patient satisfaction scores, and clinical outcomes in real time, helping leadership make data-driven decisions to improve care delivery. Dr. Michael Arcaro at Capital Health says, “[athenahealth] helps us to collect the data that’s needed for quality metrics that we have to report. That’s been a big benefit of having athena as a partner.”
ZoomCare, an innovative multi-specialty organization with 220-plus providers at more than 50 clinics, partnered with athenahealth for numerous reasons, not the least being the power of our network. As Chief Executive Officer Jeff Fee says, “We chose athenahealth because of the company’s expertise in ambulatory care, their ability to facilitate information exchange with our health system partners, and their experience improving revenue cycle performance as we scale and evolve.”
By tailoring insights and automation to the unique needs of different practice sizes, athenaOne ensures that every provider—regardless of scale—can maximize efficiency, revenue, and patient satisfaction.
The benefits physicians reap from being part of the athenaOne network
By joining the athenaOne network, physicians gain access to a powerful, data-driven ecosystem that continuously evolves to meet the needs of modern healthcare. In a nutshell, the athenahealth network helps practices with:
- More revenue – Real-time financial benchmarks help maximize reimbursements and minimize denials.
- Better patient care – Predictive analytics highlight early interventions for at-risk patients.
- Less administrative work – Automated workflows, efficient integrations and user group tips help save time.
- Continuous improvement – Data-driven best practices surfaced through insights on the network help practices close care gaps and meet increasing benchmarks for quality measures.
- Simplified connections to the healthcare ecosystem – athenahealth’s network of more than 277,000 clinical integrations with labs, imaging centers, pharmacies and more8 removes the complexity and cost of maintaining these critical connections.
- Configurable experience – With third-party solutions across 50 digital health capabilities and 60 specialties,9 the athenahealth Marketplace enables you to tailor your experience with fully integrated solutions to address your organization’s specific needs.
- Future-proofing – All software updates are included in your fees and automatically applied, allowing you to always be on the most recent version with the greatest security measures, cutting-edge technology improvements, and support.
athenaOne’s cloud-based, single-instance SaaS model provides real-time insights, automated revenue cycle optimization, and better patient care coordination — something on-premise, or restricted EHRs simply can’t match. Learn more about athenaOne’s features or see athenaOne in action yourself by requesting a demo from the button in the upper right. We can’t wait to show you what you’re missing.
* These results reflect the experience of one particular practice and are not necessarily what every athenahealth client should expect.
- Based on athenahealth data as of Dec. 2024; M010
- Based on athenahealth data for 12 months ending Dec. 2024; M171
- Based on athenahealth data as of Dec. 2024; M191
- Based on athenahealth data as of Dec. 2024; M008, M012
- Based on athenahealth data as of Dec. 2024; M017
- Based on athenahealth data for 12 months ending Dec. 2024; M016
- Based on athenahealth data for 12 months ending Dec. 2024; M225
- Based on athenahealth data as of Dec. 2024; M020
- Based on athenahealth data as of Dec. 2024; M029