How can we overcome barriers to interoperability in healthcare?
With so many benefits to interoperability in healthcare, why isn’t seamless data exchange a reality across the healthcare ecosystem in the United States? More than 15 years after interoperability of electronic health records was set as a goal in the HITECH Act, why has the vision remained elusive? And why do practitioners, institutions, and insurance companies still rely on digital faxing—a 20th century technology—to exchange crucial patient information today, even with seismic shifts in technology capabilities, including artificial intelligence?
We can all agree that healthcare interoperability is a crucial component of modern healthcare delivery, enabling the efficient exchange of patient data across different systems and clinicians. But the gulf between the current state of most interoperability in healthcare and what physicians need remains vast.
The sheer quantity of available information is one factor contributing to physicians’ frustration. According to the athenahealth Physician Sentiment Survey 2024-25, 61% of physicians said they often feel so overloaded with information that it increases their stress levels.1
Furthermore, with different healthcare IT vendors solving data exchange problems in their own ways, the lack of a unified approach to interoperability can complicate matters. The Physician Sentiment Survey also found that 95% of physicians said that getting the right clinical information at the right time is very important to them; however, only 28% said that sending and receiving patient data on a different EHR was easy.2
Numerous challenges of interoperability in healthcare affect not only the technical aspects but also policy, legal, and operational factors. In this article, we’ll look at many of the main barriers to interoperability in healthcare and suggest questions you should ask your Health IT vendor to understand their approach to interoperability.
1. Data standardization
One of the primary obstacles to interoperability is that healthcare data is not always standardized or normalized across systems. Different healthcare organizations use a variety of formats and standards for data entry, organization, and storage, making it difficult for them to exchange information.
Although standards for interoperability exist, such as HL7, FHIR (Fast Healthcare Interoperability Resources), and C-CDA (Consolidated Clinical Document Architecture) data exchange of electronic health records can be hindered by a lack of consistent adoption and implementation. Systems using incompatible standards may struggle to communicate with one another; in this situation, data may not arrive in a usable format, slowing down care delivery.
Choosing the right platform can help. Practices that implement a cloud-based SaaS platform with built-in support for HL7, FHIR, CCD, and other standardized formats are able to exchange data efficiently. Built-in integrations across diverse healthcare IT systems also help reduce EHR interoperability issues.
2. Data security and privacy concerns
Ensuring the security and privacy of patient data while enabling interoperability is another critical challenge. Healthcare data is highly sensitive, and compliance with regulations such as HIPAA (Health Insurance Portability and Accountability Act) is essential to protect patient privacy. It takes significant effort to ensure that patient data remains secure during transmission and storage.
There are also cybersecurity risks to consider. As important as it is to healthcare outcomes to be able to access and share patient data among caregivers, keeping sensitive patient information secure is not optional. Achieving both security and interoperability can be a delicate balance.
For these reasons, it’s essential to partner with an EHR vendor that has the right experience to handle patient data security and privacy on your behalf. Consider a cloud-based SaaS solution with enterprise-grade security features, including encryption, access controls, and built-in HIPAA compliance measures. A comprehensive offering like this could make it easier for practices to adhere to regulatory requirements and improve interoperability in healthcare.
3. Fragmented Health IT ecosystem
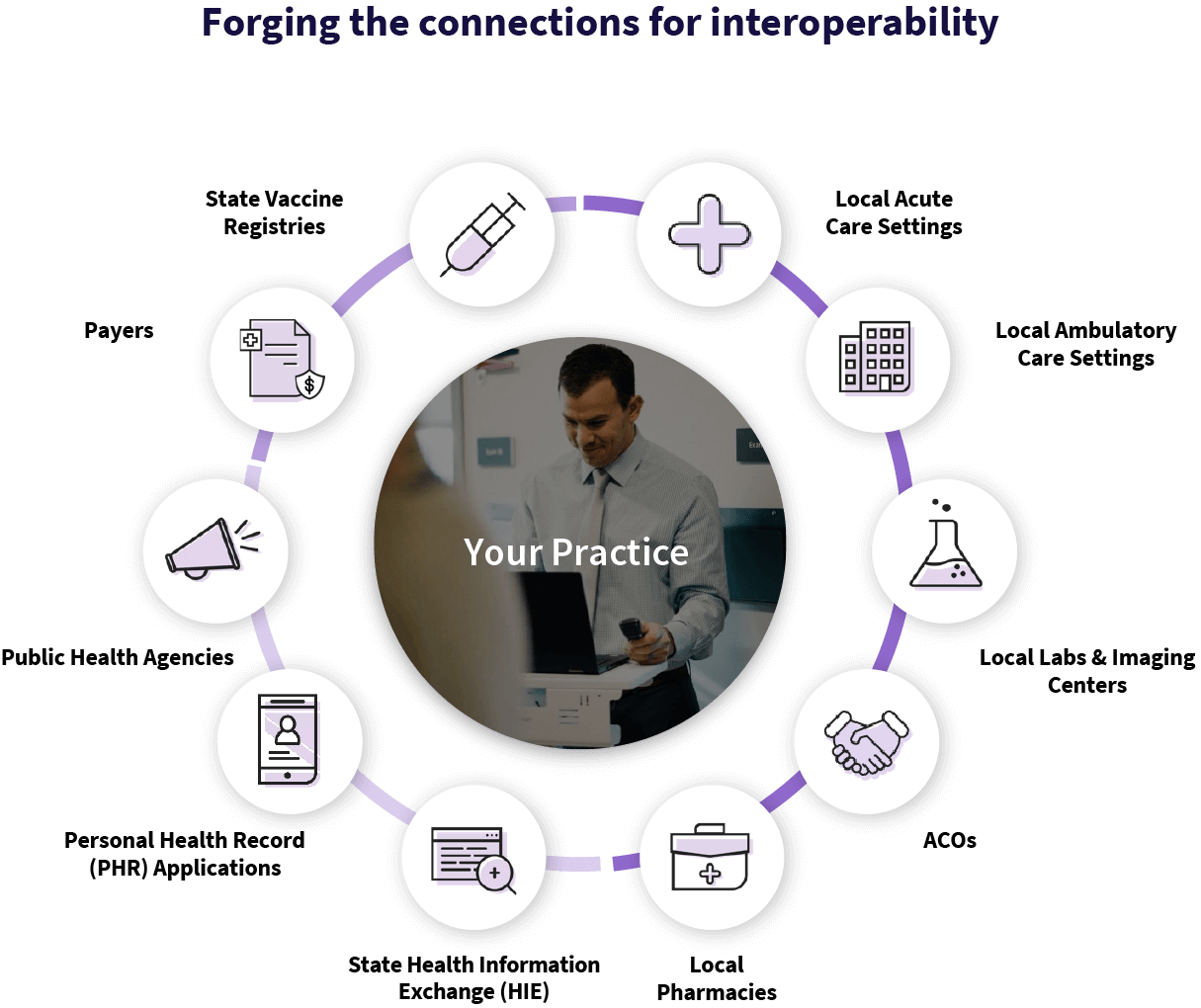
The lack of standardization in data formats has been mentioned, but that’s not the only fragmented aspect of healthcare in the U.S. The lack of a unified health IT ecosystem makes it difficult to achieve true interoperability between—and sometimes even within—healthcare systems. A single healthcare entity may use several health IT systems, often supplied by multiple vendors; and each one comes with its own database, software, and architecture.
An integrated SaaS platform can help resolve these EHR interoperability challenges. With millions of patients and a vast network of providers, a connected SaaS platform such as athenaOne® enhances collaboration between primary care physicians, specialists, hospitals, and ancillary healthcare services. Choosing one with hundreds of thousands of pre-built integrations enables interoperability between a multitude of healthcare IT vendors, reducing fragmentation and simplifying data exchange among them.
athenaOne enables real-time, cross-provider data sharing—one with established connections to Qualified Health Information Networks (QHIN) such as CommonWell and a strong commitment to the Trusted Exchange Framework and Common AgreementTM or TEFCA™.
4. Financial and resource barriers
Who is ultimately responsible for connecting a practice to the healthcare ecosystem? Traditionally, that burden lands on the practice itself, and requires both the funds and the know-how to implement. For some practices, creating integrations can feel both too expensive and too much work to be worth their while, limiting how interoperable their system can be, and sacrificing access to important external data.
Sometimes the most significant barrier to interoperability is the most obvious one: the cost. Some EHR vendors charge to set up each integration to another healthcare IT platform, which means clinicians and healthcare providers may desire more connectivity but bump up against financial constraints, especially at smaller or more rural practices. The costs involved—whether upgrading or replacing a legacy system to meet today’s interoperability standards or paying for the necessary integrations to connect with third parties plus the technology and staff to maintain those integrations—can impose a serious burden.
Furthermore, some practices may have trouble justifying the return on investment for adopting interoperable systems. While programs such as MIPS and MACRA provide some incentive, not all medical practices and providers receive sufficient financial support to make the transition. When you consider the added expense of identifying and hiring the right experts to take on the work of interoperability, the price of admission can seem insurmountable.
Taking on the full expense and responsibility of implementing an interoperable system doesn’t have to be the only way forward. A cloud-based SaaS model reduces the high upfront costs associated with on-premise infrastructure by offering subscription-based pricing that’s more predictable and manageable. With its built-in interoperability features, practices can benefit from easier health information exchange with the potential for lower associated costs.
Finally, choosing a vendor that offers the expertise to forge and maintain connections to the healthcare ecosystem can also spare practices from having to find and hire expert IT staff and/or consultants—or taking on the work themselves.
The right platform, supporting EHR interoperability solutions, enables clinicians to find what they need without adding to their cognitive overload.
5. Operational and workflow integration
For interoperability to reach its potential, it’s not adequate to simply “turn on the tap” and let the data flow. Patient data comes from many different sources—imaging centers, labs, specialists, and hospitals—and can be cluttered with information the clinician doesn’t need. Having the wrong data can lead to costly errors and delays, not to mention frustration for time-pressed physicians and clinical staff.
To spare the busy clinician from a deluge of data, steps should be taken to deliver the right patient data in the right place at the right time. That includes formatting and integrating data from multiple systems, deduplicating and removing irrelevant content, and placing it into the patient record when and where it’s needed.
The right platform, supporting EHR interoperability solutions, enables clinicians to find what they need without adding to their cognitive overload. Advanced data processing, AI-driven analytics, and intelligent formatting within the SaaS platform help organize, prioritize, and deduplicate critical patient information.
Moreover, a configurable platform that offers open API capabilities can be adapted to the way your clinicians work. API capabilities enable medical practices to tailor workflows and integrate them with existing ones.
6. Legal and regulatory barriers
While HIPAA’s federal laws regarding healthcare data sharing, privacy, and security apply to all U.S. states, each state may have its own laws that impose additional requirements. This patchwork of regulations can create confusion and make it difficult for healthcare entities to adopt consistent, interoperable practices across state lines – something needed now more than ever with the consolidation of healthcare providers and multi-specialty, multi-state affiliated practices and health systems.
In addition, concerns regarding patient consent and data ownership can complicate data exchange. Patients must be fully informed and provide consent for their data to be shared across systems; however, differing interpretations of “data ownership” can interfere with smooth data exchange.
A platform with built-in patient consent management tools makes it simpler to be in compliance. Regularly scheduled updates incorporate changes to programs such as MIPS, as well as any changes to CPT and ICD-10 codes, which can help practices comply with the latest standards.
Questions to ask your Health IT vendor about interoperability
Wondering how your Health IT vendor handles interoperability? Make sure you understand their approach to each of the above challenge areas. We’ve provided these questions as a jumping-off point to help you determine if they’re meeting best practices.
- What standards do you support for data exchange, such as HL7, FHIR, and C-CDA, and how do you ensure consistent implementation across your platform?
- How do you handle data from external providers (labs, imaging centers, etc.) that may use different formats to ensure it arrives in a usable format for clinicians?
- What built-in integrations do you offer to facilitate seamless data exchange with other healthcare IT systems?
Get to know our approach to interoperability
At athenahealth, our vision is to create a thriving ecosystem that delivers accessible, high quality, and sustainable healthcare for all. Keeping that ecosystem connected is one reason we prioritize interoperability that works.
If you’re interested in learning more about our approach to interoperability, reach out today and set up a time to connect.
1. 2025 Physician Sentiment Survey of 1,001 physicians nationwide. January 2025 fielded by Harris Poll, sponsored by athenahealth.
2. 2025 Physician Sentiment Survey of 1,001 physicians nationwide. January 2025 fielded by Harris Poll, sponsored by athenahealth.
3. Based on athenahealth data as of Dec. 2024; M020