Investment in AI innovations and automation are paying off big for practices
The administrative burden on healthcare practices is undeniable, especially when it comes to revenue cycle management (RCM). With increasing demands and complex processes, practices often find themselves buried under tasks that detract from time spent with patients and can slow payment, making it harder for smaller practices to remain independent.
Physicians are optimistic about the role that purposefully developed AI tools can play to reduce administrative burdens in healthcare. In fact, 83% of physicians surveyed said that they believe that AI could eventually alleviate many of the problems facing healthcare.1 Building on a decade of AI research and significant R&D investments, we’ve introduced AI-powered innovations designed to streamline RCM tasks with a company goal to reduce this administrative workload by 50% over the next three years.
Here are six ways athenahealth’s AI-enabled tools – integrated directly into our cloud-based healthcare technology – are making a difference for clinicians in practices from solo start-ups to large enterprise organizations.
1. Smarter insurance selection powered by AI logic
Accurate insurance selection can be one of the most time-consuming aspects of revenue cycle management. Integrated directly into athenaOne®, AI-powered insurance selection processes a picture of the patient's insurance card through a machine learning model that analyzes the image, extracts information from the card, and pairs it with patient data to recommend the correct insurance.
Tina Kelley, Director of Operations at Mountain View Medical Center, notes that automating insurance selection with this tool has reduced the administrative time spent on manually entering patient insurance information. "Automating insurance selection removes guesswork for our staff, ensures accuracy, decreases denials, and helps us get paid faster, which is essential for our growing practice."
See the difference integrated tools can make
2. Faster and more accurate claims creation
Manual charge entry can be time-consuming and increase the likelihood of errors. In 2023, athenahealth began investing in additional AI capabilities with an Auto Claim Create feature that generates claims automatically after a patient encounter. This not only helps improve cash flow by speeding up claims submission but also cuts down on the recurring administrative tasks that often overwhelm staff. Creating claims automatically can be especially helpful with high volume, repetitive claims, such as those during flu season or child wellness visits.
The Auto Claim Create feature can help reduce charge entry lag and the time it takes to submit claims to insurance. For example, from January to June 2024, athenaOne clients using Auto Claim Create had a median charge entry lag that was 66% lower than clients not enrolled in that service (2.17 days vs 6.7 days).2 Using this feature in athenaOne can help reduce time spent on claims, improve overall claim accuracy, and improve financial performance.
Explore athenaOne revenue management
3. Reducing claim denials and improving payment recovery
Denial management can take up an enormous amount of practice time and resources, but athenahealth is leveraging AI to help reduce this burden. According to a 2024 survey by Premier, nearly 15% of reimbursement claims submitted to private payers were initially denied, leading to $10.6 billion in practice time and resources spent disputing claims that should have been approved from the outset.3
athenahealth’s AI-powered rules engine helps ensure claims are accurate the first time they’re submitted. By analyzing data from over 160,000 providers on the network4, our system identifies potential claim issues in real time, allowing staff to correct errors before submission. This vast dataset also helps enable smarter decision-making, classifying claim denials and predicting the likelihood of approval upon resubmission or appeal.
athenaOne's RCM features leverage these insights from the network to help practices quickly identify and resolve potential issues that would lead to a denial in real time, before submission. This helps practices reduce the administrative headache associated with rework and improves overall financial outcomes, so they can have more confidence in the quality and efficiency of their claims. Across the network, athenaOne practices enjoy an industry-leading clean claims submission rate of 98.4%.5
AI-powered tools help identify potential claim issues in real time, allowing staff to correct errors before submission.
In addition to the AI and automation capabilities within the software, athenahealth also partners with practices to take on the burden of working claims denials. athenahealth's Enhanced Claim Resolution (ECR) service integrates seamlessly with athenaOne to manage complex and denied claims, allowing your staff time to focus on patient care.
Practices using Enhanced Claim Resolution saw a 2.3 percentage points increase in collections per visit6 and practices that also added our Medical Coding service saw a 7.6 percentage points increase compared to similar athenahealth network clients not live on these services7 thanks to decreases in denial rates, increases in effective resubmission of denials, and higher patient pay performance.
Reduce claims denials & rework
4. Streamlining prior authorization processes
Prior authorization has long been one of the most burdensome tasks for physicians and their staff. According to the American Medical Association, physicians reported they spend nearly two full days processing prior authorizations each week and 95% of physicians attributed prior authorization to increased physician burnout.8
In response, we launched Authorization Management services to automate and streamline prior authorization workflows. Practices using our services enjoy a >98% success rate in managing authorizations.9 Our prior authorization capabilities are enhanced by Authorization Prediction and Chart Analysis. These capabilities help identify prior authorization requirements and relevant chart information, improving efficiency and accuracy.
For example, South Texas Spinal Clinic has transformed its prior authorization process using athenahealth’s tools. What once took 6-8 weeks for approval can now be completed in as little as five days, reducing administrative overhead and improving financial performance.10
According to Angela Szymblowski, Director of Clinical Operations, achieving this level of efficiency without athenahealth would require six or more full-time employees. “We went down from having four people to do authorizations to one person being the gatekeeper for this platform,” said Szymblowski.
See authorization management in action
5. Streamlining clinical documentation with ambient listening technology
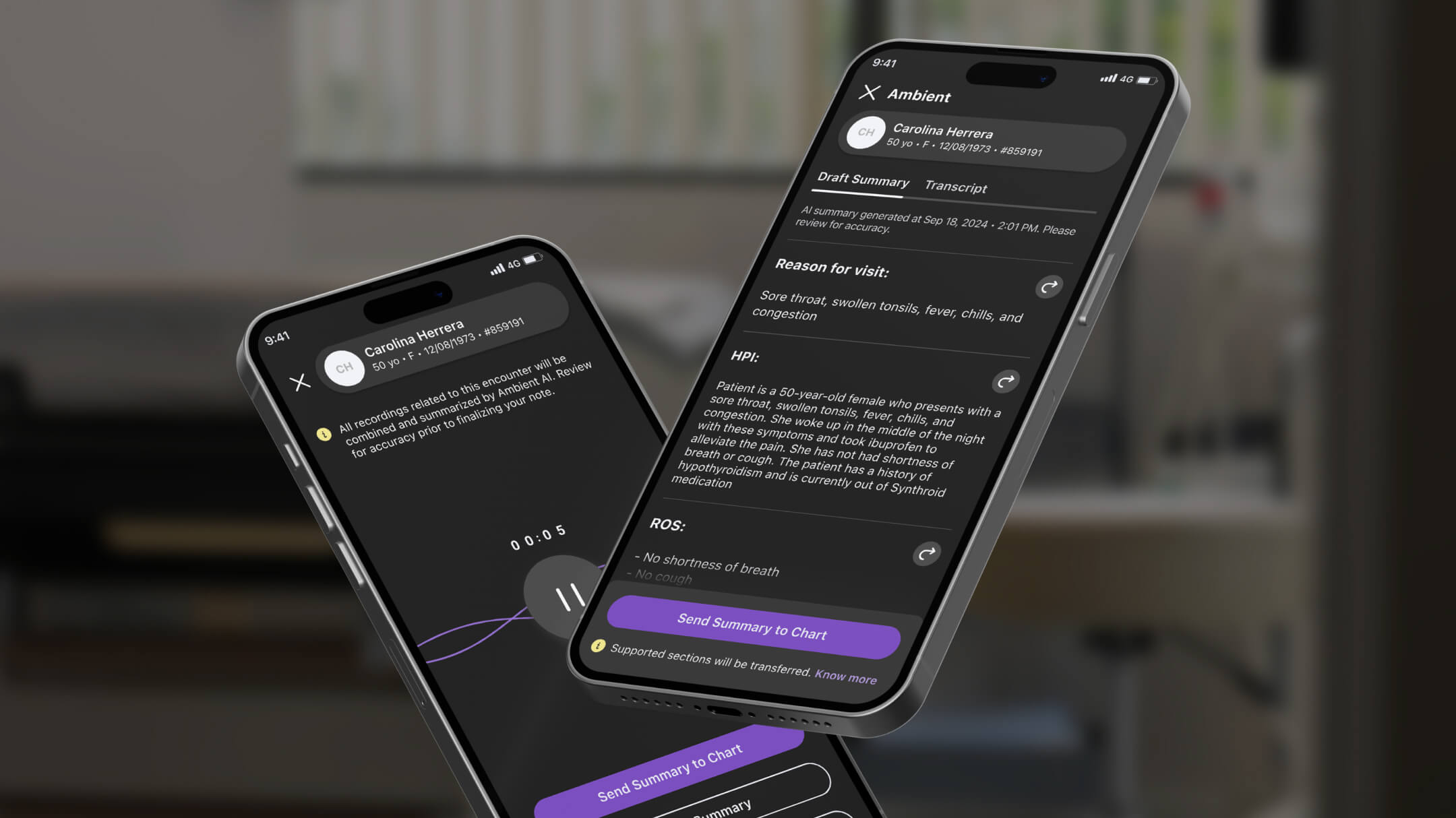
athenahealth's Ambient Notes is an AI-powered feature embedded within athenaOne Mobile that simplifies clinical documentation by recording patient visits and using generative AI to create comprehensive note summaries, which are then seamlessly integrated into patient records.
This automation allows clinicians to focus more on patient care during encounters, enhancing the overall experience for both providers and patients. Using ambient AI technology in athenaOne, one orthopedic practice saw a 40% reduction in documentation time.11 With multiple ambient models available, individual clinicians can select the one that best aligns with their specialty and documentation style, ensuring flexibility and personalization, rather than a one-size-fits-all solution.
Documenting your notes faster means you can close more patient encounters, which gets the billing process started sooner.
6. Customizable AI-powered solutions for practices’ unique pain points
athenahealth’s robust network gives practices direct access to hundreds of Marketplace Partners, including many that offer AI solutions that are fully integrated with athenaOne, streamlining your workflow and keeping you from having to open and maintain separate software.
To further tailor your athenaOne solution, select specialized apps from our Marketplace Partners built for specific workflows and pain points, such as scheduling, check-in, patient communication and voice-activated AI-assistants.
More AI-powered Marketplace apps are added monthly as capabilities increase and developers join athenahealth on this journey to reduce administrative burdens and connect the healthcare ecosystem. athenaOne practices can benefit from this flexibility and futureproofing, as well as the continued insights from the largest connected network in the US.
Explore AI assistant apps in our Marketplace
Using AI in healthcare tech to help clinicians and improve outcomes
athenahealth's AI innovations are revolutionizing how healthcare practices manage their revenue cycles. By automating tasks like insurance selection, claims creation, denial management, and prior authorization, athenahealth is helping practices reduce administrative workloads, speed up claims processing, and improve financial outcomes.
athenahealth is dedicated to fueling innovation and integrating purpose-driven AI healthcare solutions into our technology. With built-in core software updates throughout the year – driven by addressing needs surfaced from clinicians – and new AI apps built over our network to tailor your solution, practices using athenaOne can future-proof their tech stacks to continue leveraging new, powerful capabilities. Learn more about how we’re developing new healthcare AI integrations, and explore more about athenaOne.
Individual customer results may vary. The customer experience(s) referenced do not guarantee results or performance that any individual customer may experience or should expect.
1. 2023 Physician Sentiment Survey, commissioned by athenahealth and fielded by Harris Poll, Jan 2024.
2. This statistic is calculated using the Charge Entry Lag Metric Table in the Analytic Data Warehouse, and includes all clients who were active on the network during the time period (January-June 2024). Charge entry lag is reported as the median number of days it takes from an encounter start to the creation of the claim.
3. Premier. (March 21, 2024). Trend Alert: Private Payers Retain Profits by Refusing or Delaying Legitimate Medical Claims. Retrieved Feb 2025, from https://premierinc.com/newsroom/blog/trend-alert-private-payers-retain-profits-by-refusing-or-delaying-legitimate-medical-claims
4. Based on athenahealth data as of Dec. 2024
5. Based on athenahealth data for twelve months ending Mar. 2024; results compared to competitors' self-reporting of clean claim submission rates.
6. Based on a sample of 145 Small Group customers who were live before April 2022 are still live today. This does not include customers on Medical Coding. Individual customer results may vary. The results of this sample do not guarantee results or performance that any individual customer may experience or should expect.
7. Based on a sample of 85 Small Group customers from Family and Internal Medicine who were live before April 2022 are still live today. Individual customer results may vary. The results of this sample do not guarantee results or performance that any individual customer may experience or should expect.
8. AMA. (July 18, 2024). Exhausted by prior auth, many patients abandon care: AMA survey. Retrieved Feb 2025, from https://www.ama-assn.org/practice-management/prior-authorization/exhausted-prior-auth-many-patients-abandon-care-ama-survey#:~:text=They%20and%20their%20staff%20spend,of%20physicians%20feeling%20that%20way.
9. Based on athenahealth data as of Dec. 2023.
10. See case study: https://www.athenahealth.com/case-studies/south-texas-spinal-clinic
11. See case study: https://www.athenahealth.com/resources/case-studies/orthoatlanta