Women’s health is undergoing a massive shift. Historically, the scientific and clinical research into medical conditions unique to women have not been prioritized to the level of other common health conditions. On average, women spend 25 percent more time in “poor health” than men, according to research from McKinsey.1 This disparity highlights why redefining women’s health is essential.
The good news is a corrective change is underway. Women are looking for a different approach to care, and physicians are finding innovative and effective ways to deliver it. Women's health physicians are now focusing on community and economic health, not just reproductive health, for a more comprehensive picture. What’s more, research shows that every one dollar invested in women’s health unlocks three dollars in economic growth—that's a 3x rate of return.2
So, let’s dive into some of the ways that physicians have begun redefining women’s care in the U.S., and the tools they can leverage to implement these critical changes.
Women’s health physicians are focused on providing more holistic, patient-centric care
Government initiatives, legislation, and social trends have played a pivotal role in driving the movement to a more holistic view of women's healthcare. In fact, in November 2023, the Biden administration launched the White House Initiative on Women’s Health Research. The program––the first of its kind––has the ambitious goal of changing how research on women’s health is prioritized, leading to a higher standard of care for women in the U.S.3
This government initiative indicates a broader change happening in healthcare: the shift toward a more comprehensive approach to women’s care. Rather than focusing women’s healthcare on reproductive health, we’re now seeing the expansion of care to many different subspecialties, including obstetrics, gynecology, endocrinology, and menopause support.4 Women today want to receive more comprehensive care for every phase of life, and many clinics specializing in care for women are adding services to do just that.
What can women’s health providers do to support patients seeking these additional services? Let’s look at some of the pervasive challenges faced by women’s health providers today, and how the right tools and technology can help.
Women’s health––the challenges behind the change
Women have unique healthcare needs throughout their lives. But care for women has historically been disjointed at best, or narrowly focused, at worst. In reality, women stand to benefit greatly from access to healthcare services that extend beyond obstetrics and gynecology to family planning services, post-partum care, managing menopause, breast health and mammography, urogynecology, and many others. What's more, many are advocating for an integrated approach to such services, delivering a better experience to women throughout their lifetime.
This separation of specialties, along with the relative lack of medical research into women’s health topics, has led to significant care gaps. Today, 4 out of 5 women in the U.S. go undiagnosed with a women’s health condition.5 Without better coordination, even common conditions are slipping through the cracks.
And while women and their care providers face unique challenges, they also share challenges faced by the industry at large: patients want more access, flexibility, and convenience. Care providers need to deliver excellent, patient-centric care while contending with the often overwhelming clinical and administrative work needed to operate day-to-day.
The good news is that technology-enabled tools and services are now available to address many of these challenges so providers can do more with less. And, due to the paradigm shift mentioned above, women’s health providers have an excellent opportunity to apply technology to better serve their patients and save time.
What does that look like in practice? Let’s look at some of the most effective tools and services being employed today and how women’s health providers can make the most of them.
Using personalization to enable patient-centric care for women
In some ways, the shift toward a more holistic approach to women’s health is all about patient-centricity. Addressing your patients’ health needs at every stage of their lives means more effective and coordinated care from one stage of life to the next, along with more convenience and accessibility for your patients.
The technology you use to run your practice has a real impact. For instance, healthcare IT solutions are adding functions to help physicians stay more focused on their patient, especially during the moment of care. With the right platform, you can leverage AI-enabled dictation services so you’re able to spend more focused time with your patient, and follow-up documentation is more efficient and accurate.
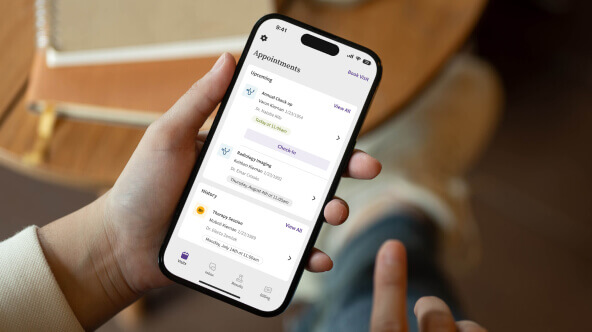
The right healthcare tech will also offer communication and engagement tools in the form of a patient portal or patient app. Empowering your patients to communicate with their care team and access their own health information creates a stronger bond between patient and physician, and helps your patients feel more involved with their own care. As an added benefit, it also creates efficiencies for your staff by mitigating certain time-consuming, manual processes like managing scheduling and facilitating communication.
Providing better care should be proactive, too. Your healthcare IT solution should enable you to engage patients based on profile information, so you can recommend visits for services like breast cancer screenings or other age- or demographic-specific procedures.
Expand access to care with telehealth and virtual care services
Telehealth has been a big story in healthcare in recent years, super-charged by the COVID-19 pandemic. Embracing this platform for certain types of appointments, such as prescription updates and chronic disease management, has been hugely beneficial for patients and providers alike.
Telehealth can add significant value for women’s health providers in particular. One of the most obvious benefits is flexibility––telehealth provides your patients with more options when they need access to your services, and often means they’ll be able to see you sooner. This flexibility can be especially crucial for patients with limited mobility, or those who are managing chronic symptoms from conditions like polycystic ovary syndrome (PCOS) and endometriosis. Telehealth can also make it more convenient for caregivers or family members to join appointments when needed.
Offering telehealth can also be a boon for business. Incorporating telehealth services can enable you to expand your patient population and maintain schedule density throughout the week.
Look for a healthcare IT solution with embedded, HIPAA-compliant telehealth capabilities. The right platform will make scheduling and participating in telehealth appointments both comfortable and convenient for patients and providers.
Enabling a patient-centric approach to care with VBC
Across US healthcare, an increasing number of practices are starting up value-based care (VBC) programs or shifting greater emphasis to their existing VBC programs. In fact, it’s estimated that by 2027, 43 million more lives will be in VBC models compared to 2022.6 That’s a massive reshaping of the payment model landscape the industry is built around, and women’s health providers and their patients stand to benefit as much (or more) than anyone.
Part of what’s driving this change is the benefit to patients. Value-based models are meant to realign the interests of patients and physicians to reward better health outcomes, cost-effective techniques, and improved patient access.
Practices using a VBC or hybrid model need tools that will allow them to proactively identify care gaps and track the ever-evolving regulatory requirements behind certain quality programs. The right healthcare IT solution should work to help your practice succeed under any payment model so you can provide the highest quality of care while also maximizing revenue.
Strategic interoperability to create a comprehensive view of care
Physicians need to be able to see their patients' detailed medical histories outside their own clinic. This is especially important for women’s health services, as women have historically depended on a wider variety of specialists for different needs and at different times in life.
Your healthcare IT solution should include connected EHR capabilities to help create a single source of truth when it comes to care coordination between yourself and other providers. With the right solution—one that exchanges data with other care centers—you can pull up your patient’s electronic chart to see clinical data from external care settings incorporated into your workflows, giving you seamless access to health information like diagnoses, lab results, prescriptions, and more that enable you to offer an even higher level of care.
Utilizing a solution that proactively surfaces relevant patient information with ease can also provide numerous efficiencies for you and your staff, automating a number of previously manual tasks like retrieving lab and imaging reports and requesting health records.
Your healthcare IT solution is the foundation for transformation
As women’s care becomes more patient-centric, so can your practice. The right technology partner can help you stay focused on patient care and personalization, expand access and flexibility to your patients, find new or greater success with alternative payment models like VBC, and get a more complete, holistic view of your patients’ health so you can coordinate with other physicians and close more care gaps. By selecting the right technology, you can deliver the high-quality care, convenience, and ultimately better health outcomes your patients deserve.
Learn more about how athenaOne can help physicians deliver more holistic care for women.
1McKinsey & Co., Closing the data gaps in women’s health; https://www.mckinsey.com/industries/life-sciences/our-insights/closing-the-data-gaps-in-womens-health; IS125
2Ibid
3The White House, Launch of White House Initiative on Women’s Health Research; https://www.whitehouse.gov/gpc/briefing-room/2023/11/17/launch-of-white-house-initiative-on-womens-health-research/
4American College of Obstetricians and Gynecologists, “Subspecialties of Ob-Gyn", 2024; https://www.acog.org/career-support/medical-students/medical-student-toolkit/subspecialties-of-ob-gyn
5McKinsey & Co., Closing the data gaps in women’s health; https://www.mckinsey.com/industries/life-sciences/our-insights/closing-the-data-gaps-in-womens-health; IS125
6McKinsey & Company, Jan 2024, What to expect in US healthcare in 2024 and beyond, https://www.mckinsey.com/industries/healthcare/our-insights/what-to-expect-in-us-healthcare-in-2024-and-beyond?stcr=FEFACC03D40F492EBD8401B5DCEEB6C3&cid=other-eml-alt-mip-mck&hlkid=2d8461c861f644cdb13cae55b6af9283&hctky=14669808&hdpid=edd3998f-a0c6-45fa-86c6-b0cd71574e4d; IS079