Alyssa M. Degnan, D.O.
A solo practitioner lessens administrative tasks, boosts financial results
athenaOne’s Extended RCM services eases coding burdens, leads to higher revenue
Post-Covid claims backlog
Overwhelming coding needs
Inefficient prior billing service
Delayed collections, decreased income
Administrative burnout
athenaOne
athenaOne® Medical Coding
athenaOne® Enhanced Claim Resolution
athenaOne® Authorization Management
Insurance Detection
athenaTelehealth
Results
"Collectibles have gone up and we're making more money because we have more patients, but we're also making more money because the monies are being collected more efficiently."
39%
reduction in days in accounts receivable
59%
reduction in back-end denial rate
95%
Overall collection yield increased from 87%
As is the case with many sole practitioners, Dr. Alyssa M. Degnan was inundated with medical coding responsibilities on top of serving a full panel of patients at her internal medicine practice in Aiken, S.C. The result was long, frustrating evenings and weekends dealing with entry lags, claims denials, error messages, and, worst of all, delayed payments from insurers and patients.
Dr. Degnan had embarked on her own in 2018 after many years of association with another medical group, and her young practice grew rapidly during the Covid pandemic — “quicker than we could swallow water,” as she put it. She needed to hire and train staff, manage a large base of Medicare patients, and handle a growing waiting list. She spoke of those demands as “Herculean startup challenges.”
“We were learning coding on the fly at night-time after hours when I was already tired from seeing patients all day,” said the doctor of 22 years. “We felt like our backs were against the wall.” Her finances were also suffering, “We lost a lot of money at the end of the first year.”
With athenaOne Medical Coding, collections go up and denials go down
In 2022, after a poor experience with her first medical billing service, she adopted athenahealth’s full suite of billing, coding, and claims resolution solutions, including upgrading to athenaOne’s Extended Revenue Cycle Management (ERCM) services. Since then, she said, the improvements have been extraordinary across the board.
“Collectibles have gone up and we're making more money because we have more patients, but we're also making more money because the monies are being collected more efficiently,” she said. Indeed, an analysis of Dr. Degnan’s first-year success with ERCM shows a reduction of days in which claims sit unprocessed in accounts receivable, from 28 to 17; a denial rate reduction from 4.4 to 1.8 percent; and a 95 percent overall collection yield, up from 87 percent.
Dr. Degnan first became an athenaOne customer in 2018 to address what she described as a “very challenging” rate of denials for billing and referrals. “We opened with 350 patients in 2018 and within 24 months we were the number one or number two fastest-growing MDVIP practice in the country,” she said. With work mounting, she added, she felt her practice needed more help handling administrative demands.
Decreased revenue and unnecessary claim swirl with her previous billing service led to frustration provider burnout
In 2022, she reached back out to her athenahealth Customer Success Manager to discuss her additional needs. She said she wanted to feel confident she was submitting clean claims from the start, and putting an end to unworked claims and missed filing deadlines. Most of all, she wanted her financial performance to improve so she could expand into areas like Chronic Care Management, a revenue stream she was missing out on because of time lost to medical red tape.
“There is no way we ever could have even thought about doing that when we were using our older billing and coding service,” she said. That third-party service, she explained, was mishandling claims, inputting errors, and leaving hold buckets and denials unaddressed for up to 72 hours. “I would drop the claim, they would correct the claim, the coder would make a mistake,” and she would have to readdress the claim herself.
More income, lighter administrative duties and improved efficiency allows for more focus on care and growth opportunities
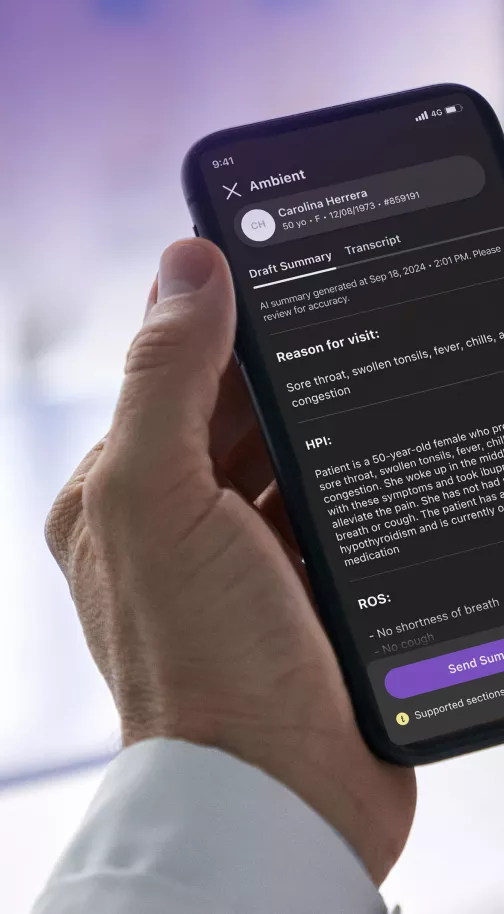
Going live with the athenaOne Advanced suite of services allowed Dr. Degnan and her staff to put billing and coding in the hands of athenahealth’s HIPAA-compliant and certified coding teams. Those teams are third-party audited to ensure accuracy, compliance, and efficiency; and they provide ongoing support to resolve time-consuming and complex claims and to manage denials.
“There's peace of mind now when I come in the next day and I look at the buckets that they're being worked,” she said. “The simplicity of the athena coding service and the quickness and efficiency of how they scrub the claim and get the claim dropped — it's much more efficient. The process moves very quickly compared to our prior experience.”
Would she recommend athenaOne services to others? Approached by a colleague seeking advice on opening his own practice, Dr. Degnan said: “My response to him, which was honest and true, was that it was the best EMR that I had ever used in my 22 years of practice. And then I encouraged his group as well to sign on for the Advanced billing services because we saw such a dramatic improvement in our own collections.” Dr. Degnan added that her partnership with athenahealth allows her to collect revenues without the cost, time, and effort of training new and existing staff in coding duties. It also allows her to pay her team more and grant them — and herself — more free time. “They can have more time off,” she said, “and a happy staff leads to better health care.”
“When we keep our patients happy, they keep coming back,” she said, noting that many of her longtime patients qualify for Medicare. “It means [they are] invested in me and my staff, and it just continues to breed long-term success for the sustainability of a small practice when 72% of practices are bought out by corporations or hospitals.
*These results reflect the experience of one particular organization and are not necessarily what every athenahealth customer should expect.