Resource Center
All ContentBlogCase Studies
- athenahealth
- March 11, 2025
- 9 min read
10 ways patient engagement tools enhance healthcare
From scheduling to billing and care coordination, these patient engagement tools help patients and practices thrive. Read moreYou may also like

- Christy Maerz
- March 18, 2025
- 6 min read
Revenue Cycle Management
6 ways to measure healthcare revenue cycle performance
Discover how to measure and track financial performance with these crucial RCM metrics.
Read more 
- Chad Dodd
- March 28, 2025
- 6 min read
athenahealth Products
AI, interoperability, HIT partnerships take the stage at HIMSS 2025
Missed seeing us at HIMSS in March? Chad Dodd recaps our AI innovations, powerful partnerships, and more.
Read more 
- Nele Jessel, MD
- March 25, 2025
- 7 min read
athenahealth Research
Insights from the 2025 Physician Sentiment Survey
Physician optimism is increasing but issues persist in data exchange and more. Get insights from our annual survey.
Read more 
- Christy Maerz
- March 20, 2025
- 7 min read
Revenue Cycle Management
Get crucial RCM metrics for better practice management
Discover how Insights Dashboards enable your practice to quickly and accurately measure performance.
Read more 
- Christy Maerz
- March 18, 2025
- 6 min read
Revenue Cycle Management
6 ways to measure healthcare revenue cycle performance
Discover how to measure and track financial performance with these crucial RCM metrics.
Read more 
- Chad Dodd
- March 28, 2025
- 6 min read
athenahealth Products
AI, interoperability, HIT partnerships take the stage at HIMSS 2025
Missed seeing us at HIMSS in March? Chad Dodd recaps our AI innovations, powerful partnerships, and more.
Read more 
- Nele Jessel, MD
- March 25, 2025
- 7 min read
athenahealth Research
Insights from the 2025 Physician Sentiment Survey
Physician optimism is increasing but issues persist in data exchange and more. Get insights from our annual survey.
Read more 
- Christy Maerz
- March 20, 2025
- 7 min read
Revenue Cycle Management
Get crucial RCM metrics for better practice management
Discover how Insights Dashboards enable your practice to quickly and accurately measure performance.
Read more 
- Christy Maerz
- March 18, 2025
- 6 min read
Revenue Cycle Management
6 ways to measure healthcare revenue cycle performance
Discover how to measure and track financial performance with these crucial RCM metrics.
Read more Empower your practice

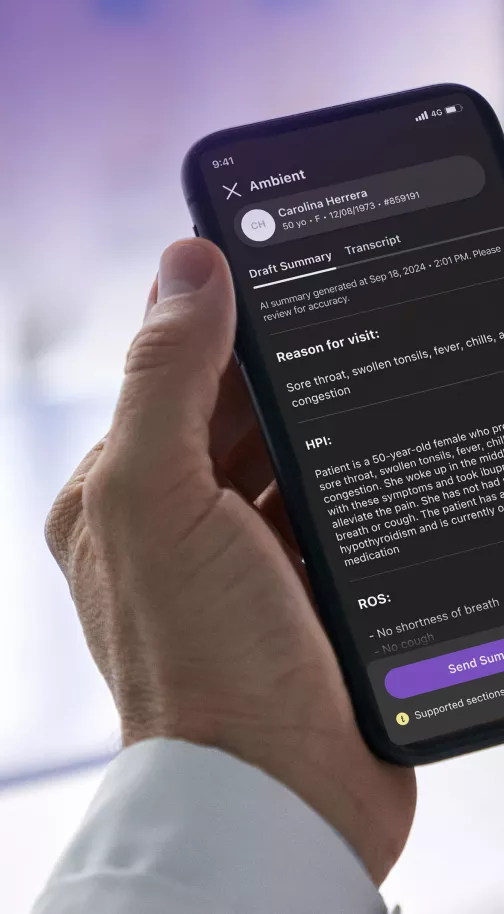
AI powered patient engagement
Learn how AI tools can help improve patient loyalty and outcomes.