MIPS PY2022 Results: athenahealth providers outperform national averages
Data from the 2022 Performance Year (PY2022) under the Merit-based Incentive Payment System (MIPS) has been released, and clients using athenahealth’s athenaOne® platform considerably outperformed national averages across nearly all MIPS metrics in the aggregate and by practice specialty. 2022 was the first year that cost, comprising 30% of a composite score, had a significant impact on scoring.1
Below are some key findings from this year’s MIPS results so you can see how athenaOne® providers compared to their national peers.
What are the MIPS healthcare program measures and what do they mean?
MIPS is a vital component of the Quality Payment Program (QPP) established by the Medicare Access and CHIP Reauthorization Act (MACRA). This program focuses on value-based care (VBC) by linking payment for services to the quality and cost-efficiency of care. Eligible clinicians report data across four categories: Quality, Improvement Activities (IA), Promoting Interoperability (PI), and Cost, and they receive a composite score that determines their future MIPS payment adjustment. In 2024, eligible clinicians received MIPS payment adjustments based on their performance in 2022.
Providers earn payment adjustments for Medicare Part B services based on their performance compared to an annual threshold set by the Center for Medicare & Medicaid Services (CMS). For Performance Year 2022 (PY2022), the composite score threshold for providers increased 15 points to 75.2 Medicare Part B payment adjustments can be positive for providers who perform above the threshold, neutral for those at the annual threshold, or negative for those performing below the threshold.
Providers who perform best on these measures receive higher revenue for achieving the higher results, including positive payment adjustments (up to 9% for PY2022).3 Tracking and performing well on MIPS quality measures has a material effect on a practice’s bottom line and is an indicator of how well a provider improves the health outcomes of patients while managing the overall cost of care.
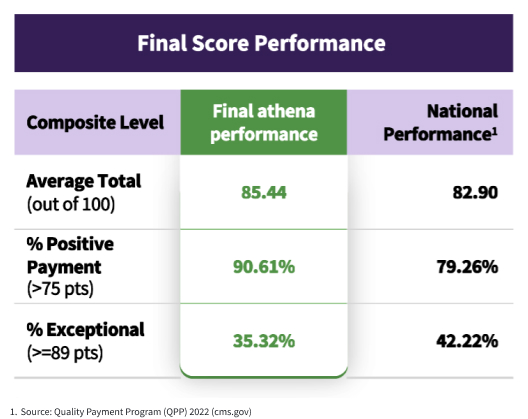
Here are the key findings from the 2022 MIPS performance year (the most recent data available):
1. Overall athenahealth client MIPS performance outshines the nation by 11.35%
- athenahealth clinicians with positive payment adjustments: 90.61%4
- National rate: 79.26%
More users of athenaOne for MIPS reporting5 received positive payment adjustments for Medicare Part B in 2024 than their peers using other EHR, practice management, and patient engagement systems across the country.
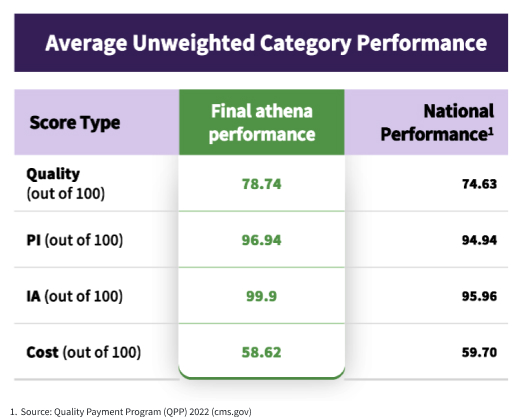
2. Exceptional MIPS Quality scores for athenaOne clients
The Quality category is critical, as it accounts for 30% of the overall MIPS score. Quality category metrics focus on outcome, appropriate use, patient safety, efficiency, patient experience, and care coordination.
- athenahealth average Quality score: 78.74
- National average: 74.63
athenaOne’s EHR system proactively optimizes both the Quality and PI categories on behalf of providers. During the Quality optimization, athenahealth uses network insights and scaled automation to identify additional MIPS measures that will strengthen Quality category performance, and, in turn, lead to higher MIPS positive payment adjustments.
3. athenaOne users achieved above average Promoting Interoperability scores
The Promoting Interoperability (PI) score is 25% of the composite score for 2022 and reflects how well a provider’s Certified Electronic Health Record Technology (CEHRT) such as athenaOne shares information with other physicians, clinics, hospitals, pharmacies, and labs to enable coordinated care the reduces duplication, improves efficiency, and provides a more holistic view of a patient’s health.
- athenahealth average PI score: 96.94
- National average: 94.94
Enhanced clinical workflows for prescription drug monitoring embedded within athenaOne contribute to these superior results, as does athenaOne’s singular comprehensive solution that combines the Electronic Health Record (EHR) software with medical billing, revenue cycle and practice management and patient engagement capabilities and connects clinicians to 160k+ providers on the athenahealth network.6
athenaOne providers have access to 165k+ clinical integrations (total connections to labs, imaging centers, pharmacies, patient record sharing networks, HIEs and registries)7 and automatic connections to 86k care sites in CommonWell and Carequality, leading to impressive interoperability that gets results.8
4. Impressive Improvement Activities performance
- athenahealth average IA score: 99.90
- National average: 95.96
Most providers using athenahealth’s EHR achieve full points in this category without extra effort, thanks to athenaOne’s diverse measurement portfolio, intuitive performance dashboards and library of Clinical Guidelines.
5. Specialty-specific MIPS success in primary care
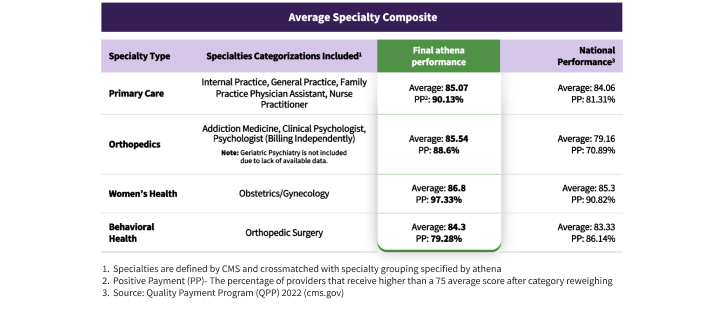
- athenahealth primary care clinicians achieving positive payment: 90.13%9
- National rate: 81.91%
- Average Composite score: 85.07 (athenahealth) vs. 84.06 (national)
6. Strong MIPS results for behavioral health providers
- athenahealth providers’ average composite score: 84.30
- National rate for behavioral health providers: 83.33
- Behavioral Health providers benefit from targeted Quality measures.
7. Outstanding MIPS performance by OB/GYN providers
- athenahealth women’s health clinicians achieving positive payment: 97.33%
- National rate for OB/GYN providers: 91.23%
- Composite score: 86.80 (athenahealth) vs. 85.39 (national)
8. Orthopedics providers achieve MIPS excellence
- athenahealth orthopedics clinicians achieving positive payment: 88.60%
- National rate for orthopedists: 70.89%
- Exceptional performance rate: 38.26% (athenahealth) vs. 34.44% (national). Exceptional performers earn an additional positive payment adjustment for performing above the exceptional threshold.
How athenaOne helps providers achieve superior MIPS performance
athenahealth’s primary product and suite of services, athenaOne® helps providers document, monitor, and submit MIPS program data. By using information captured during patient encounters to inform program performance reports, providers know throughout the year how they are performing and can make adjustments that improve quality measures – without a separate software program to use and maintain or another interface to open.
athenaOne features that help providers succeed with MIPS
athenaOne includes these standard features designed to help clinicians achieve leading positive payment rates:
- embedded MIPS program requirements in the patient chart and visit surfaced during typical clinical workflows to help identify care gaps at the point of care
- improvement insights from the integrated MIPS Dashboard, built to track all CMS program specifications
- performance optimization, including step-by-step suggestions to address gaps that are informed by CMS requirements as well as data from across the athenahealth network
- rolling performance analysis, ensuring the highest performing 90-day period is submitted for PI category scores
- automated submission to CMS for the Quality, PI, and IA categories, saving clinicians time and easing the administrative burden of attestation
- comprehensive MIPS documentation, education, and support available from the athenaOne Success Community and dedicated Customer Success Managers, including 1:1 coaching.
MIPS Reporting & Quality Program Support with athenaOne
The Performance Year 2022 MIPS results illustrate that athenahealth providers excel across multiple key quality measures and clinical specialties, setting a high standard for performance in the healthcare industry and outperforming their national peers on multiple MIPS metrics. With higher positive payment adjustments, superior category scores, and specialty-specific successes, providers using athenaOne consistently demonstrate their commitment to delivering high-quality care and achieving financial success.
athenaOne is a comprehensive electronic medical records (EMR), practice and revenue cycle management, and integrated patient engagement software and services suite that helps providers succeed in the MIPS Quality Payment Program. athenaOne's robust features, including care coordination tools, streamlined reporting and advanced analytics, allow doctors, clinicians, and practice managers to review progress toward quality program measures throughout the year and to benchmark their performance against others across the network.
By choosing athenaOne, providers can optimize their MIPS performance by delivering quality-focused care that both improves patient outcomes and minimizes administrative burdens. Want to learn more? Request a demo and see how athenaOne can help boost your MIPS performance.
More MIPS and APM resources
Continue exploring
- Source: Quality Payment Program (QPP) 2022 (cms.gov)
- Source: Quality Payment Program (QPP) 2022 (cms.gov)
- Source: Quality Payment Program (QPP) 2022 (cms.gov)
- Positive Payment (PP) - The percentage of providers that receive higher than a 75 average score after category reweighing
- Eligible athenaOne clinicians are defined as clinicians who: (1) actively used athenaOne during the reporting period, (2) were enrolled in athenahealth’s MIPS program, (3) were eligible for MIPS based on CMS’s eligibility API, and (4) permitted athenahealth to submit their MIPS data
- Based on athenahealth data as of Dec. 2023; M020
- Based on athenahealth data as of Dec. 2023; M020
- Based on CommonWell reporting of 36K+ care sites connected to athenahealth (www.commonwellalliance.org) and Carequality reporting 50K+ care sites connected to athenahealth (https://carequality.org) as of July 2024
- Specialties are defined by CMS and crossmatched with specialty grouping specified by athenahealth 3Source: Quality Payment Program (QPP) 2022 (cms.gov)