Resource Center
All ContentBlogCase Studies
- Maury Brown
- December 12, 2024
- 6 min read
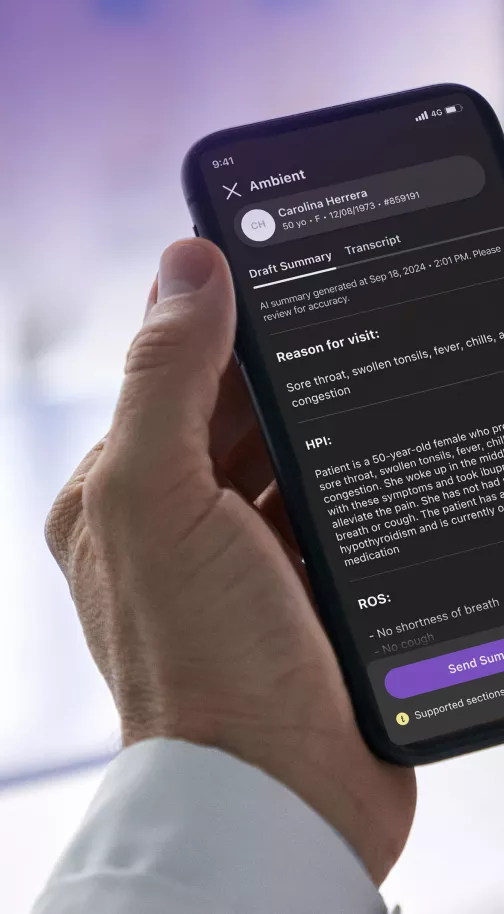
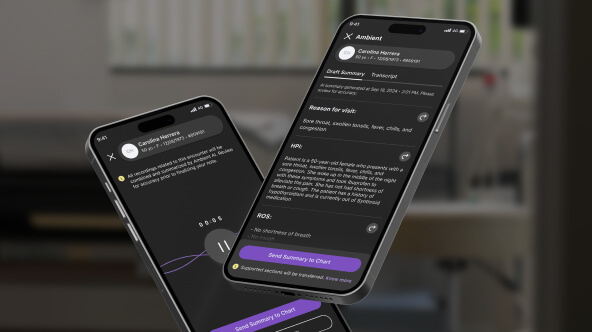
Manage your patient communications inbox without burning out
As a physician, you know that keeping patients engaged and satisfied is crucial for their health outcomes. Regular and timely communication plays a key role in improving patient adherence to treatment plans, ensuring they follow through with medication regimens, attend necessary appointments, and understand their diagnoses. In fact, consistent
Read more